Much more concern and confusion now centres on HRT (hormone replacement therapy), which is composed of synthetic versions of the ‘female’ hormones, oestrogenOestrogen is one of the main female sex hormones…. and progesteroneProgesterone is one of the main female sex hormones….. The apparent panacea turned out to have a dark side, when HRT was found to actually raise the risk of heart disease and breast cancer following the large Women’s Health Initiative study in 2002.1 This has left millions of women in their forties and fifties in a dilemma. Do you plump for the benefits of HRT and hope to avoid the side effects? Or do you stay off it and hope to find something else? Official medical advice is that short-term use – two years – is not linked with an added risk. Even so, many have stopped taking it. In the wake of the 2002 study, the number of prescriptions in the UK and in the US has halved. In the years since there has also been a significant decline in the number of breast cancers.2
Natural vs Synthetic Hormones
There is a solution that is widely used in the US but little known in the UK. It involves the same hormones found in regular HRT but they come in a subtly different form known as ‘bio-identical’, which means that they are exactly the same as the ones your body was making until it reached the menopause, or the andropause in the case of men. The ones used in HRT are not identical, and this is very probably the reason for the problems they have caused; for example, a type of oestrogen still widely used (over 500,000 prescriptions were issued in England alone in 2010) is known as conjugated oestrogen and comes from the urine of pregnant mares, so it contains types of oestrogen normally only found in horses. The best-known brand is Premarin, and this was used in the Women’s Health Initiative trial.
The replacement for progesterone that is used in regular HRT is known as progestin (or progestagen), and the best-known brand is Provera. It also has a significantly different chemical structure from progesterone. This is linked to the very different effects the two have: progesterone is the hormone made in large amounts during pregnancy, it is also a diureticA diuretic is a substance that increases the amount of urine produced and therefore makes you urinate more frequently…., and it decreases the risk of blood clots, has antidepressant effects and helps to build bone. Progestins can cause miscarriages, fluid retention and blood clots, and it is linked with mood swings and can reduce bone density.
Hormones Decline with Age
The fact is that hormone levels do often decline dramatically later in life. TestosteroneTestosterone is a male sex hormone important for sexual and reproductive development…. deficiency can result in lack of sex drive, lack of motivation and depression in both men and women. Lack of oestrogen results in vaginal dryness and lack of progesterone, from which all these hormones can be made, results in lack of everything. Also, progesterone dampens down adrenal hormones so a common effect of progesterone deficiency is more anxiety, bursts of anger, insomnia, tight and aching muscles, all of which are often found in the menopause.
As you can see from the diagram below progesterone is the ‘mother’ of all hormones, itself made from cholesterol. (Beware statin enthusiasts – driving down cholesterol too low eg below 3.5mmol/l could lead to hormone deficiency.)
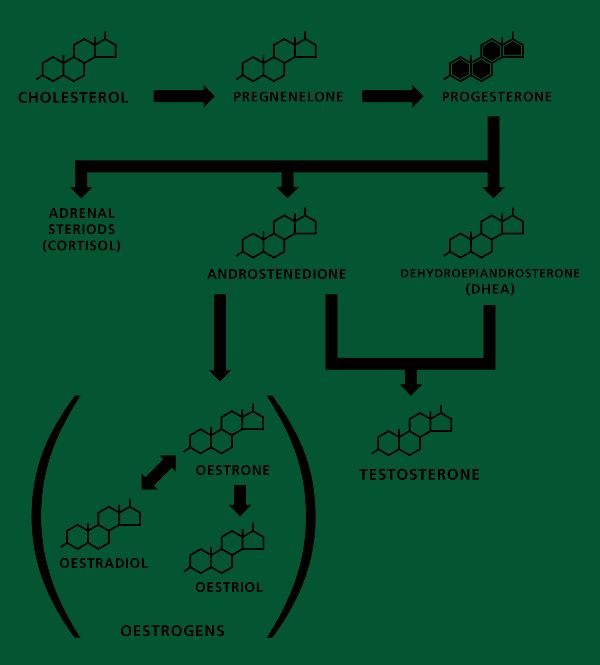
The body will always make cortisolCortisol has been nicknamed ‘the stress hormone’ as it is released in higher levels during the body’s flight or fight response to stress. Levels of… – the stress hormone – in preference to anything else because it is to do with our immediate survival. This may not actually be the case when you get stressed watching the news but your body thinks it is so. Consequently, DHEA levels go low. The more stressed you are the higher the cortisol and the lower the DHEA, until you are completely burnt out in which case both go low. This in turn means that there is less DHEA to manufacture testosterone. Chronically low amounts of DHEA is one of the consistent indicators that you are ageing faster than your chronological age, which is why it has become a popular supplement.
DHEA – do you need it?
DHEA is the most abundant hormone in the body, but production for both men and women peaks at age 20 and it is reduced to half that rate by age 40, and by the time you are 65 you will only be producing 10–20 per cent of your youthful level. It’s part of the pathway that produces the sex hormones, so it is likely to have an impact there and it is also the hormone that balances cortisol, the stress hormone. This means that low levels can reduce the effectiveness of the immune system, which becomes less responsive when you’re stressed. So there is certainly a logical case for restoring your levels. DHEA supplements benefit mice, but there is not yet any hard proof that they slow down ageing in humans.
Symptoms of a deficiency include:
- Feeling burnt out
- Unable to cope with stress
- Insomnia
- Lack of drive or motivation
Your body naturally produces 35–60mg of DHEA a day, which can be accurately measured in both saliva and blood. Practitioners are likely to prescribe between 15mg and 50mg. If you are taking DHEA, you should then re-check your level after about 90 days. I sometimes recommend it to people who are burnt out for one month only, at a dose of 25mg.
The other way to increase your DHEA level is to reduce your stress and so bring down your cortisol level. Some very simple exercises that can do this have been developed by the HeartMath Institute (see my report on HeartMath They are designed to eliminate negative thought loops and to promote sustained positive emotional states. In one study with 45 volunteers, the 15 who did the exercises for a month saw their cortisol drop by 23 per cent, and their DHEA level increase by 100 per cent.3 They also reported feeling much less stressed and more positive. There was no change in the others.
Progesterone
Many hormone experts think that all post-menopausal women should be on physiological levels of progesterone, because none is produced by the ovaries after the menopause and your body uses it to make all the rest of the hormones. It is needed to protect your bones: stimulating the bone-building osteoblasts while oestrogen damps down the demolition team of the osteoclasts. In fact, it could be that progesterone plays a larger role in bone protection than oestrogen. Women who have periods when no progesterone is produced – known as anovulatory – start to lose bone mass;4 however, the results from trials using progesterone to protect bones have been contradictory; for example, one found that it was four times more effective than oestrogen HRT, with none of the associated risks,5 whereas two more found no effect, although menopausal symptoms, such as hot flushes and night sweats, were reduced.6
Could you be deficient? These are the symptoms to watch out for:
- Anxiety, depression, irritability and mood swings
- Loss of bone mass/increased risk of osteoporosis
- Increased pain and inflammation
- Insomnia
- Decreased HDL cholesterolHDL is short for high density lipoprotein. It is the “good cholesterol” responsible for removing harmful cholesterol from the bloodstream. High HDL levels reduce the…
- Excessive menstruation
If you have two or more positive answers you could well benefit from seeing an expert. But how can you be certain that you won’t be at the same risk of cancer as women taking HRT? You can’t be absolutely certain, but there is evidence that combining oestrogen with progesterone is considerably safer than the progestin– oestrogen combination. Inevitably, randomised trials haven’t been done, but there is a very interesting natural experiment underway in France where both progestins and progesterone are widely used, because some women prefer one and some the other.
Researchers have followed over 80,000 women to see what happens to those in each group, and the result was a convincing win for progesterone, which caused no increase in cancer. Those getting the progestin combination, however, had their risk raised by 69 per cent. Taking oestrogen alone raised the risk by 29 per cent.7
The oral progesterone used in France, is now licensed in the UK for treating the menopause – called Utrogestan. Doctors can also prescribe Pro-juven, a transdermal progesterone cream, as an unlicensed medicine.
Oestrogens
During middle age, a woman’s level of the three oestrogen hormones begins to decline, because these hormones are no longer needed to prepare the womb lining for pregnancy. One effect of this is that menstrual flow becomes lighter and often irregular, until eventually it stops altogether. Other signs of a declining level of oestrogen include:
- Thinner, older skin with more wrinkles
- Vaginal dryness
- Increased risk of urinary tract infections
- Decreased sex drive
- Loss of bone mass
Once again, if these seem familiar, you could benefit from being checked out. Even if your oestrogen level is low, you could still be suffering from a condition called ‘oestrogen dominance’, symptoms of which include water retention, breast tenderness, mood swings, weight gain around the hips and thighs, depression, loss of libido and cravings for sweets. This seems counterintuitive, but it’s because oestrogen and progesterone need to be kept in balance. So if you are in your forties and having anovulatory periods, you could be in a state of oestrogen dominance, even though your oestrogen is low, because your progesterone levels are even lower.
The result can be too many growth signals to the cells of the breast and womb, raising the risk of cancer. This is why you need a good practitioner. Just replacing low oestrogen without checking what else is going on might not make you feel better and could lead to cancer.
To complicate matters further, you don’t just replace ‘oestrogen’. It comes in three varieties – oestrodial, oestrone and oestriol. And, furthermore, they are present in very different proportions. Oestriol is the weakest, and pre-menopausal women normally have lots of it; it makes up about 90 per cent of the total amount. The next most abundant is oestradiol, the most potent one, at around 7 per cent, followed by oestrone at 3 per cent.
Bio-identical practitioners will test to find the proportions of your oestrogens and then prescribe accordingly. ‘I often find that estrone levels are elevated in post-menopausal women,’ says Dr Gluck ‘while estradiol and oestriol are too low.’ More than half her patients are prescribed progesterone along with a combination of bio-identical oestradiol and oestriol.
Testosterone
Although testosterone is also present in women, it is men who experience most of the problems when levels are low. In women it is strongly linked to lack of sex drive and often given in small doses by bio-identical hormone practitioners.
Just as the decline of oestrogen and progesterone lead to many of the key signs of female ageing, falling testosterone does the same for men. In both cases there is a decline in sexuality, along with thinning bones, thickening waists, fading memory, emotional swings, aching joints and night sweats.
According to Dr Malcolm Carruthers, who has compiled a number of surveys, around a fifth of men over the age of 50 complain about a loss of potency, sex drive and morning erections, along with mild to moderate depression, irritability and an earlier-than usual decline in memory and concentration. And yet the idea that this forms some kind of syndrome comparable to the menopause – otherwise known as the andropause – is too frequently dismissed out of hand by most doctors.
Another hormone that is often deficient is the thyroid hormone thyroxine. ~I have written extensively about this here.
In conclusion
Hormones affect almost every part of your system so, not surprisingly, when your levels drop too low you can suffer a confusingly wide range of symptoms – and most of these could also be caused by something else! If you’ve been suffering from any of the following for a while, it’s worth having your hormones checked to see if they could be contributing:
• Anxiety, depression, irritability and mood swings
• Increased pain, inflammation and aching joints.
• Insomnia, night sweats and weight gain
• Thinner, older skin with more wrinkles
• Decreased libido and lack of energy and drive
• Confusion and memory problems
Depending on your symptoms and test results, there may be real benefit in correcting the hormones you are deficient in by using bio-identical hormones given in the dose equivalent to that which your body would normally make. I recommend that you are reassessed after three and six months, because some hormone imbalances will be corrected so that you won’t need to keep taking as much. Will natural hormones extend your healthy lifespan? The odds are good, but there’s no definitive proof yet.
To find out more read my book The 10 Secrets of Healthy Ageing.
References
- J. E. Rossouw, et al., ‘Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the Women’s Health Initiative randomized controlled trial’, Journal of the American Medical Association, 2002;288:321–33
- S. Tehillah, et al., ‘Rates of Atypical Ductal Hyperplasia Have Declined with Less Use of Postmenopausal Hormone Treatment: Findings from the Breast Cancer Surveillance Consortium’, Cancer Epidemiol Biomarkers Prev, 2009:2822–2828; doi:10.1158/1055–9965.EPI-09–0745
- R. McCraty, et al., ‘The impact of a new emotional self-management program on stress, emotions, heart rate variability, DHEA and cortisol’, Integrative and Physiological and Behavioral Science, 1998;33(2):151–70
- J. Prior, et al., ‘Spinal bone loss and ovulatory disturbances’, New England Journal of Medicine, 1990;323(18)1221–7
- J. Lee, ‘Osteoporosis reversal: The role of progesterone’, International Clinical Nutritional Review, 1990;10:384–91; see Also J. Lee., ‘Osteoporosis reversal with transdermal progesterone’, Lancet, 1990;336(8726):1327
- A. Cooper, et al., ‘Systemic absorption of progesterone from Progest cream in postmenopausal women’, Lancet, 1998;351(9111):1255–6
- A. Fournier, et al., ‘Unequal risks for breast cancer associated with different hormone replacement therapies: results from the E3N cohort study’, Breast CancerRes Treat, 2008;107(1):103–11

Comments
Join the Conversation on our Facebook Page