Domain 1 – Eat a Low Glycemic Load (GL) Diet
Keeping blood glucose levels in the low-normal range is reflected by a low glycosylated haemoglobinHaemoglobin is the protein that is found in red blood cells. It contains iron and is responsible for carrying oxygen from the lungs to the… (HbA1C) which is associated with reduced risk for dementia in several studies.(17) Type 2 diabetes almost doubles risk for dementia.(18) Diabetes is also associated with more rapid brain shrinkage.(19) Even people in the upper normal range of blood glucose have increased brain atrophy, impaired cognition and increased risk of dementia.(20)
For instance, one trial measured HbA1c and glucose levels in several thousand elderly people over the course of almost seven years.(21) In that time, over a quarter of the participants developed dementia and the rising glucose levels were associated with an 18% increased risk of dementia in those without diabetes and 40% in those with or who developed diabetes.
But even more important than loss of glucose control is the loss of insulinInsulin is a hormone made by the pancreas. It is responsible for making the body’s cells absorb glucose (sugar) from the blood…. control. Back in 2004, researchers at Columbia University stated that people with high insulin levels – the principal hallmark of metabolic dysfunction – were twice as likely to develop dementia as those with healthy levels. Moreover, those with the highest insulin levels had the worst memories.(22) The same year, an Italian study also established a link between heightened insulin levels and declining mental function. (23) Similarly, a Puerto Rican study found that people who consumed large amounts of sugar doubled their risk of suffering poor cognitive function,(24) while another US study discovered a strong correlation between blood sugar level and memory loss.(25) Two studies – one in Ireland (26) and the other in the United States (27) –established a link between high dietary glycemic load (GL) and cognitive decline. Indeed, both of these reports suggested that high GL is even more predictive of the pathological changes associated with Alzheimer’s than either high carb or high sugar intake. A high GL diet is also associated with more amyloid plaque (28) and cognitive decline, especially in those with the ApoE4 gene.(29) A long-term study found evidence that brain shrinkage and impaired cognition is more common among people with high blood glucose levels, even within ‘non-diabetic’ limits.(30) This cognitive decline starts young. Cognitive decline in overweight children is associated with a high GL diet (31) and adolescents with metabolic dysfunction driven by a high GL diet have been shown to have shrinkage of the hippocampal area of the brain and cognitive deficits (32, 33).
“Those who ate the healthiest diet had an 88% decreased risk of developing dementia and a 92% decreased risk of developing Alzheimer’s disease.”
In practical terms this means avoiding sugar as much as possible and eating fewer carbohydrates and, when you do, eating ‘whole’ carbohydrateCarbohydrates are the primary source of energy for the body as they can be broken down into glucose (sugar) more readily than either protein or… foods such as wholegrain bread or pasta and oat cakes since the fibreFibre is an important part of a balanced diet. There are two type of fibre; soluble and insoluble. Insoluble fibre helps your bowel to pass… in these foods helps ‘slow release’ the sugars. Eating white bread is associated with a poorer cognitive test performance, whereas high fibre bread is associated with better performance.(34) Eating carbohydrate foods with proteinProteins are large molecules consisting of chains of amino acids. Proteins are essential nutrients for the human body – they are a building block of…, for example brown rice with fish, or porridge oats with seeds, or fruit with nuts, further reduces the glycemic load (GL) of a meal. Best fruits in this respect are berries, cherries and plums. These kinds of foods are consistent with a Mediterranean diet which has also been shown to reduce risk.(35) A Scandinavian study compared those with a healthy versus unhealthy diet, including the above criteria, in mid-life for future risk of developing Alzheimer’s disease and dementia 14 years later. Those who ate the healthiest diet had an 88% decreased risk of developing dementia and a 92% decreased risk of developing Alzheimer’s disease.(36)
Domain 2 – Up Brain Fats
DHADHA is short for Docosahexaenoic Acid. It is an essential omega-3 fatty acid found in fish such as salmon, mackerel and herring, and is often…
The omega-3 fatThere are many different types of fats; polyunsaturated, monounsaturated, hydrogenated, saturated and trans fat. The body requires good fats (polyunsaturated and monounsaturated) in order to… docosahexaenoic acid (DHA) is the most abundant polyunsaturated fat in the brain, concentrated in the grey matter and synapses.(37) DHA is incorporated into membrane phospholipids, where it affects the properties of the membrane, for example, maintaining membrane fluidity. DHA, along with the other omega-3 fats (EPAEPA is short for Eicosapentaenoic Acid. It is an essential omega-3 fatty acid found in fish such as salmon, mackerel and herring, and is often… and DPA) and their mediators are involved in a wide variety of processes in the brain, such as making neurons, synaptic connections, and the regulation of inflammation.(38)
Fish, especially cold-water oily fish, contain high levels of EPA and DHA and epidemiological studies consistently show that an elevated fish intake is associated with decreased risk of neurodegenerative diseases such as Alzheimer’s disease. (39, 40) Recent estimates suggest that worldwide many populations are currently consuming DHA and EPA at levels well below the recommendations issued by many international authorities (GOED), with blood levels estimated to be low to very low for most of the world, which may increase global risk for chronic disease (41).
DHA supplementation appears to show the greatest promise, particularly in the early stage before the onset of memory loss symptoms (42), and at levels at or above 1000 mg per day (43). Interestingly, positive association have also been found between walnut consumption and cognitive performance (44). Walnuts are a source of the omega-3 fat alpha-linolenic acid (ALA) and also a range of antioxidants.
Phospholipids
Phospholipids, rich in eggs and seafood, are abundant in the brain. They become attached to omega-3 DHA in neuronal cell membranes, a process that requires methylationMethylation is what occurs when the body takes one substance and turns it into another, so that it can be detoxified and excreted from the…, dependent on B vitamins which play a key role in generating DHA enriched phosphatidyl choline (PC) (45), which is one type of phospholipid.
Another phospholipid, phosphatidylserine (PS), has been found to be low in post-mortem samples from Alzheimer’s disease patients46 Interestingly, phosphatidylserine supplementation may benefit cognition in the elderly (47) but as PS is highly enriched with DHA (Kim et al. 2014), it is currently unclear whether the potential beneficial effects of PS on cognition are due to the intact PS or DHA. Phosphatidylethanolamine (PE) is also enriched in DHA, whereas much lower levels are found in phosphatidylcholine (PC) and phosphatidylinositol (PI) (48) Although PC is not highly enriched in DHA, higher plasma concentrations of PC-DHA are associated with reduced risk of dementia and AD (49), and post mortem samples from AD show depletion of PC-DHA in grey matter (50).
A number of trials have investigated the effects of providing multi-nutrient supplements containing a range of nutritional factors with the aim of supporting phospholipid biosynthesis. For example, a combination supplement containing DHA, EPA, and uridine monophosphate, choline, vitamins B, C and E and seleniumWhat it does: Antioxidant properties help to protect against free radicals and carcinogens, reduces inflammation, stimulates immune system to fight infections, promotes a healthy heart,…, has shown promise in those with MCI51.
Vitamin DWhat it does: Helps maintain strong and healthy bones by retaining calcium. Deficiency Signs: Joint pain or stiffness, backache, tooth decay, muscle cramps, hair loss….
The primary source of vitamin D is exposure to sunlight. Seafood provides the most dietary vitamin D. Supplements of vitamin D can be derived from animal or fungal source (mushrooms and yeast). Vitamin D helps neurotransmission and exerts anti-inflammatory and neuroprotective activities within the brain
Domain 3 – Keep Your HCY Low with B Vitamins
B vitamins are essential for many aspects of brain function. They are essential for healthy methylation, which is needed to build brain cell membranes and neurotransmitters that pass messages between brain cells. Hence B vitamins, especially B6, B12 and folate, are essential for the brain’s structure, ‘talking’ and ‘listening’. When in short supply, blood levels of homocysteineHomocysteine is an amino acid found in the blood. Elevated levels of homocysteine have been associated with narrowing and hardening of the arteries, an increased… go up, indicating faulty methylation.
Treatment with B vitamins later in the disease process, in those diagnosed with AD, has shown modest benefit in those in the mild stage but not in those with moderately severe AD.(67)
B vitamins and Omega-3 are synergistic
Dr Jerneren at Oxford University analysed the data from the previous VITACOG study but divided the participants into those with a high, medium and low blood level of omega-3 at the start of the trial. Those with low omega-3 status showed no beneficial effect from the B vitamins while those with high omega-3 showed a 73% decrease in rate of brain shrinkage down to that seen in healthy elderly who do not develop dementia. (68) Those with a high omega-3 status showed the largest cognitive benefits to B vitamin treatment.(69)
Two trials in China on people with mild cognitive impairment have shown slowing of cognitive decline in those given folic acidWhat it does: Critical during pregnancy for the development of a baby’s brain and nerves. Also essential for brain and nerve function. Needed for utilising… and B1270 or with a combination of folic acid and the omega-3 fatty acid DHA. (71)
These studies suggest that Hcy-lowering B vitamins can, at least, slow cognitive decline in people with a raised Hcy level over age 50 and those over 70 with Mild Cognitive Impairment and may also slow cognitive decline in those with mild AD, but not in moderate to severe AD.
Homocysteine is both a marker and a cause of brain damage
Three reviews confirm the growing evidence supporting raised Hcy levels as a likely primary predictor and cause of the brain damage that identifies AD.72 35 40 Hcy and its derivatives are neurotoxins and indicate disrupted methylation, which leads to raised levels of amyloid and tau proteins and associated plaques and neurofibrilliary tangles found in the Alzheimer’s brain. Raised Hcy leads to increased oxidative stress, brain damage and impaired circulation.
Both high homocysteine (Hcy) and low folate and B12 levels increase risk for Alzheimer’s disease (AD). (57, 58) The higher the Hcy and the lower the folate and B12 the greater is the rate of cognitive decline. (56)
An International Consensus Statement in 2018 concluded that moderately raised plasma total Hcy (> 11μmol/L), found in half of those over age 70 (59), is a main cause of age-related cognitive decline and dementia. (60) Two major meta-analyses of hundreds of studies conclude that raised Hcy is one of the best evidenced risk factors for AD and accounts for around a fifth of all risk61.(62)
Homocysteine-lowering B vitamin treatment
Hcy can readily be lowered by supplementation with B vitamins (63). Randomised Controlled Trials
In those over 50 with raised Hcy (>13μmol/L), but not diagnosed with cognitive impairment, supplementing folic acid (0.8mg/d) for three years resulted in a significant improvement in cognition compared to placebo (the FACIT trial) (64).
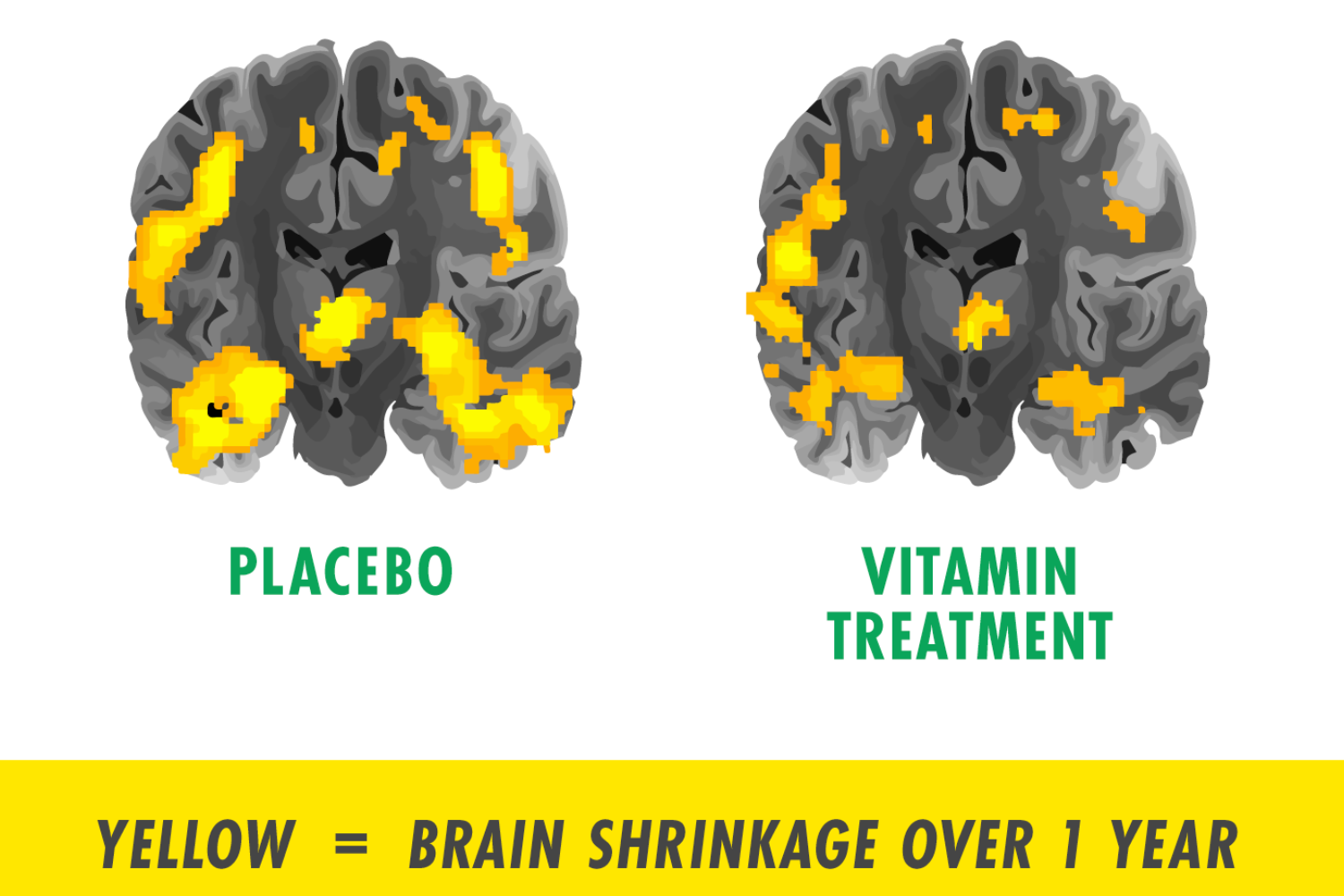
The VITACOG trial on people with Mild Cognitive Impairment by Professor David Smith and his group of the OPTIMA Study at the University of Oxford, showed that Hcy above 11 μmol/L, correlated with accelerated brain shrinkage and cognitive decline. Those given daily folic acid (0.8mg/d), vitamin B12 (500 μg/d) and B6 (20mg/d) had a significant 30% reduction in the rate of brain shrinkage versus placebo4 and almost a nine-fold reduction in shrinkage of the medial temporal lobe, which is a key area of the brain that shrinks in AD.(65) In addition, the B vitamins slowed cognitive and clinical decline. (66) (see image, used with permission from Douaud. (42) Yellow denotes area of significant atrophy).
Vitamin D deficiency increases risk of AD.(53) In a study in France involving 912 elderly patients followed for twelve years, a total of 177 dementia cases (124 AD) occurred: 25(OH)D deficiency was associated with a nearly three-fold increased risk of AD.54 Supplementing 800iu (20mg) a day for 12 months has been shown to improve cognitive function.(55)
Domain 4 – Eat and Drink Anti-Ageing
Antioxidants & Polyphenols
Antioxidants and polyphenols are plant-based nutrients that protect the brain. The older you are the more your brain needs to disarm harmful oxidants, the toxic by-products of the brain’s energy creation, and to reduce inflammation. Smoking (73) and long-term exposure to polluted air (74) are significant risk factors for Alzheimer’s dementia.
The more fruit and vegetables a person eats the lower is their risk of cognitive decline (75) with vegetables being particularly protective. (76) The best kinds of vegetables are carrots, cauliflower, broccoli, Brussels sprouts, cabbage, spinach and mushrooms. The best fruits are berries, especially blueberries and strawberries. (77, 78) Polyphenols, found not only in fruit and vegetables, but also in tea, especially green tea, red wine and the cacao in dark chocolate, are associated with preserving memory (79, 80) and a number of mechanisms exist to explain their positive actions on cognitive performance. (81) Olive oil is also promising in this regard.(82) The most protective effect is found eating six servings (500g) a day of fruit and vegetables.(83) Those in the top fifth of consumption of these kind of foods and drinks have half the risk of dementia.84 A randomised controlled trial found cognitive improvement with a Mediterranean style diet with extra virgin olive oil or nuts.(85)
A number of key vitamins, as measured in food and in the blood, correlate with decreased risk. These include vitamin C86, both in food and supplements (87) and vitamin EWhat it does: Acts as an antioxidant, protecting cells from damage, including against cancer. Helps body use oxygen, preventing blood clots, thrombosis, atherosclerosis. Improves wound… in supplements.(88)
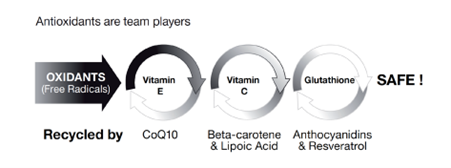
In a population study it was found that those taking supplements of both vitamin CWhat it does: Strengthens immune system – fights infections. Makes collagen, keeping bones, skin and joints firm and strong. Antioxidant, detoxifying pollutants and protecting against… (1g) and vitamin E substantially reduced risk of developing Alzheimer’s disease compared with those not taking these two supplements; either supplement on its own was not protective.(89) Vitamin E was found to be beneficial in mild to moderate AD by slowing decline of cognition.(90) A study supplementing vitamin E and selenium was not found to be protective. N-acetyl cysteine91, a precursor of glutathione, Co-enzymeQ1092 and resveratrol93, found in red grapes, is also neuroprotective.
These nutrients, together with anthocyanidins in blue/red foods and beta-carotene in orange foods are team players in disarming harmful oxidants that age the brain, however they also have roles when acted on by the gut microbiome producing secondary metabolites involved in liver function, detoxification and cell signalling with anti-inflammatory effects supporting brain function, as well as reducing cardiovascular risk and hence supply of nutrients and oxygen to the brain.(94)
Domain 5 – A Healthy Gut is a Healthy Brain
A healthy gut is essential for a healthy brain. In recent years it has become establish that there are many ways in which the gut communicates with the brain, and vice versa. This includes the production in the gut of neurotransmitters including serotoninSerotonin is a hormone found naturally in the brain and digestive tract. It is often referred to as the ‘happy hormone’ as it influences mood…., dopamineDopamine is a neurotransmitter (chemical messenger) found within the brain. It has a variety of influences on brain function including playing a role in regulating…, noradrenaline and GABA which directly influence the brain; the gut’s ability to absorb critical brain-friendly nutrients such as vitamin B12; its role in controlling inflammation and eliminating potential brain-damaging toxins; and role of the gut microbiome – the balance of trillions of bacteria that populate our gut.
Two gut-related predictors or Alzheimer’s – periodontal disease and lack of stomach secretions required for vitamin B12 absorption – illustrate this microbiome -gut-brain connection.
Having periodontal (gum) disease, a consequence of infection and dysbiosis, is associated with a significant increase of cognitive decline (95) with increasing dental visits correlating with Alzheimer’s. (96)
Decreasing production of stomach acid, required for vitamin B12 absorption, is a common occurrence in those over age 50. Two in five over 61 have low blood levels of B12.97 Gastritis98, irritable bowel syndrome (IBS) (99),gut infections such as H.pylori (100), long term use of PPI antacids (101, 102) and antibiotics103 have all been implicated or associated or with increased risk of cognitive decline and dementia.
The intestinal gut barrier functions much like the blood brain barrier, ideally allowing nutrients to pass while rejecting toxins and ant-nutrients. The integrity of the gut barrier is affected by alcohol, gliadin (104) in wheat, a lack of antioxidants and anti-inflammatory omega-3 fats which influence the microbiota (105). Gut inflammation may play a role in cognitive decline.(106)
The role of the microbiome in the gut affecting cognition is a new frontier for research.(107, 108) A study giving aged rats a faecal transplant from young rats showing significant changes in cognition (109) illustrates the potential role for probiotics, prebiotics and diets that promote a healthy microbiome.
While there is little clinical trial evidence yet there is a growing body of evidence that restoring gut health and eating a digestion friendly diet is correlated with and likely to be beneficial for protecting cognition.(110)
Domain 6 – Exercise and Keep Physically Active
Movement is one of the most powerful ways to reduce of risk cognitive decline. In fact, brisk walking was the first activity that was shown to increase the size of the hippocampus – the area of the brain critical for memory – in older adult humans! (1) In that study, participants who were randomised to walk briskly for 40 min three times per week saw an increase in the size of the hippocampus compared to a control group after a year. Participants started with the 10 minutes of walking, increased it by 5 minutes every week. In addition to walking, almost any exercise can improve brain health, and one of the ways it does that is through the production of brain-derived neurotrophic factor (BDNF).(2) Exercise particularly helps improve the amount and quality of sleep we get, (3) and decreases inflammation, (4) both of are critical factors in long- term brain health.
Resistance training or weight training also improves brain health and cognitive function in several ways. Improving strength and muscle mass is associated with better function of brain white matter – the areas of the brain responsible for making fast connections between brain areas or between the brain and the body. (5) Other studies have shown that loss of muscle mass is associated with lower brain volume and dementia, (6) and muscle mass was also positively correlated with cognitive function in individuals from the UK biobank study.(7) Only four sets per week of resistance training, which can be done in a few minutes, is enough to see benefit.(8)
The final important area of movement and dementia risk is movements that involve coordination or balance. A recent meta-analysis suggested that exercise involving coordination are the best at improving cognitive function. (9) For instance, one study showed that participants who did dance-based exercise saw greater improvements in the size of the hippocampus.(10) You could even combine resistance and coordination movements by doing something like yoga or pilates.
Domain 7 – Keep Yourself Socially and Intellectually Active
Research indicates that individuals who keep their minds active exhibit better cognition.
Social participation predicts psychological outcomes in later life. Social participation with others, particularly within friendship groups, is incrementally more important for mental well-being as people age. Older adults are at particular risk of becoming lonely, and loneliness is associated with impaired cognition and poor psychological and physical health in older adults. (108). Loneliness is strongly correlated with negative health outcomes and premature death, to a similar extent to what is seen with other risk factors, such as obesity and smoking. (109-115)
Research suggests that bilingualism and multilingualism may help to prevent memory loss in older adults. Individuals who are bilingual exhibit better cognitive function and reserve. Additionally, bilingualism has been associated with lower incidence of AZ and enhanced ability to increase learning and memory.
Neuroprotective benefits of bilingualism have been demonstrated even in individuals who have taken up language learning later in life, as just four months of language learning has been associated with improved cognitive function in older adults. (116-126)
Domain 8 – Sleep and Calm
A meta-analysis of studies on sleep found that disturbed sleep increases future risk of dementia. Combining 23 studies insomnia was significantly associated with 27% higher risk of cognitive disorders.(116) Those getting too little (six hours or less) or too much (over 8 hours) had greater risk.
Potentially beneficial interventions include meditation and mindfulness, which has been shown to lessen depression in those with dementia (118); heart rate variability (HRV) biofeedback which has been shown to lessen depression, anxiety, and improve attentional skills as well as sleep quality and stress management in older adults.(119); yoga having beneficial effects on cognitive functioning, particularly on attention and verbal memory possibly through improved sleep, mood, and neural connectivity.(120); and improved social interactions with facilitated meeting and discussion groups being associated with improved cognition and increased brain volume.(121)
References
All statement and studies can be found at www.foodforthebrain.org/AIPrefs
Food for the Brain’s AIP manifesto PDF.
Join the Campaign!
Join Food for the Brain’s campaign to prevent Alzheimer’s! Here’s how.
1. Spread the word – Alzheimer’s is Preventable. Read and share the Food for the Brain manifesto – foodforthebrain.org/aipmanifesto
- get diagnosed early to help prevent Alzheimer’s in the future
- tell all your friends over 40 to do the test too
- through this test, be part of the research project to help prevent Alzheimer’s for future generations. We are aiming for one million people! We can then chart changes in the Dementia Risk Index score and your Cognitive Function Test score. This will allow us to research and improve how to better effect positive behaviour change.


Comments
Join the Conversation on our Facebook Page