Diagnosis
Osteopaths can diagnose fibromyalgia by testing and detecting designated sensitive points on the body (see Figure 22 below). For reasons that are not yet understood, it appears to affect five times as many women as men. When considering a diagnosis of fibromyalgia it is very important to distinguish it from fibrositis, which is characterised by the inflammation of muscles or connective tissue.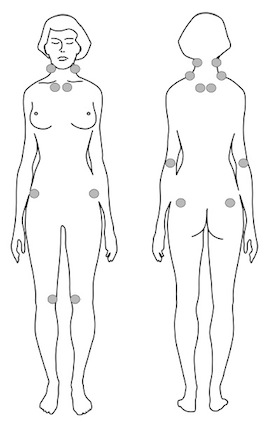 Figure 22 The cause of fibromyalgia does not stem from inflammation. Rather, research indicates that the painful muscles are due to decreased energy production and the reduced ability of muscles to relax [1]. This has been linked to a deficiency in the energy molecule ATP which is normally produced in each cell of the body to provide the fuel for its functions [2]. Without ATP, the cells (and consequently the muscle, organ or whatever tissue they are part of) cannot function optimally. In the case of fibromyalgia, the muscles fail to relax properly once they have contracted.
Figure 22 The cause of fibromyalgia does not stem from inflammation. Rather, research indicates that the painful muscles are due to decreased energy production and the reduced ability of muscles to relax [1]. This has been linked to a deficiency in the energy molecule ATP which is normally produced in each cell of the body to provide the fuel for its functions [2]. Without ATP, the cells (and consequently the muscle, organ or whatever tissue they are part of) cannot function optimally. In the case of fibromyalgia, the muscles fail to relax properly once they have contracted.
One factor contributing to ATP deficiency is a poor oxygen supply to cells. Insufficient oxygen (called hypoxia) results in low energy production and compromised cellular function in general. The disrupted sleep patterns experienced by many fibromyalgia sufferers can contribute further to exhaustion and anxiety. Studies done in France found that people diagnosed with fibromyalgia have low levels of serotoninSerotonin is a hormone found naturally in the brain and digestive tract. It is often referred to as the ‘happy hormone’ as it influences mood…. in the brain [3]. Serotonin is a neurotransmitterA neurotransmitter is a chemical messenger that carries signals between body cells. They are various types of neurotransmitters which play a major role in everyday… that is partly responsible for bringing about restful sleep. It is made from the amino acid tryptophan. Supplements of 5-hydroxytryptophan (5-HTP), in doses of 200mg one hour before bed, can help restore restful sleep.
In studies 5-HTP has very successfully reduced muscular symptoms as well. [4], [5] According to Professor Federigo Sicuteri from the University of Florence, an expert in this area of research, ‘In our experience, as well as in that of other pain specialists, 5-HTP can largely improve the painful picture of primary fibromyalgia’. [6] Like many disorders, it’s best to treat fibromyalgia on several levels – mechanical, chemical and emotional.
So-called ‘mechanical’ methods of treatment (such as massage and exercise) do help to increase the supply of oxygen to tissues by stimulating the blood flow. These do not, however, address the underlying cause of the energy deficiency and pain. Indeed, some people feel worse after massage, and many feel unable to take any exercise while they are exhausted and in pain.
Some of the most successful results have come from treating fibromyalgia on a more chemical level. Research has shown that a deficiency in magnesiumWhat it does: Strengthens bones and teeth, promotes healthy muscles by helping them to relax, also important for PMS, important for heart muscles and nervous… can lead to an increased perception of pain. [7] This in turn increases stress which stimulates the release of stress hormones. One effect of these is to push magnesium out of cells, further depleting stores of this vital mineral [8], worsening muscular pain and also putting sufferers at risk of other magnesium deficiency symptoms such as cardiovascular problems. In this way, a vicious circle of action and reaction can be set in motion. The good news is that the cycle can be broken – researchers in the US suggest that it is possible to reverse ATP deficiency due to insufficient oxygen by taking magnesium and malic acid. [9]
They report that some FM sufferers have a significant reduction in pain after as little as 48 hours. Other nutrients that are particularly necessary for the efficient production of ATP are B vitamins, manganeseWhat it does: Helps to form healthy bones, cartilage, tissues and nerves, stabilises blood sugar, promotes healthy cells, essential for reproduction and red blood cell… and co-enzyme Q10. Indeed, symptoms of a deficiency in B vitamins, particularly B1, do resemble those of fibromyalgia. Some people with vitamin DWhat it does: Helps maintain strong and healthy bones by retaining calcium. Deficiency Signs: Joint pain or stiffness, backache, tooth decay, muscle cramps, hair loss…. deficiency get wrongly diagnosed with fibromyalgia. [10] Manganese is also needed for various hormonal processes that lead to thyroxine output. Thyroxine is responsible for determining metabolic rate, so any reduction in it could lead to an overall decline in metabolismMetabolism is a term that is used to describe the chemical reactions that take place within the body’s cells. The body gets the energy it… and energy production.
Fibromyalgia, chronic fatigue and homocysteine
A team of researchers headed by Dr Bjorn Regland at the Institute of Clinical Neuroscience at Sweden’s Goteborg University ran a battery of tests on fibromyalgia sufferers, including homocysteineHomocysteine is an amino acid found in the blood. Elevated levels of homocysteine have been associated with narrowing and hardening of the arteries, an increased….
By far the most significant finding was that every single patient with fibromyalgia had high homocysteine. They also found a direct correlation between their B12 status and the severity of their reported symptoms. [11] Fibromyalgia sufferers should be routinely tested for homocysteine, and if high, immediately started on a homocysteine-lowering programme. For more information on homocysteine and related conditions, read my book The Homocysteine Solution, co-written with Dr. James Braly.
In summary, the following advice may provide relief from the symptoms of fibromyalgia:
• Eat a healthy diet, with plenty of magnesium-rich foods such as green vegetables, nuts and seeds.
• Supplement key vitamins and minerals – magnesium and malic acid (magnesium malate), vitamin B complex, co-enzyme Q10 and a multivitamin/mineral that contains manganese.
• Supplement 5-HTP, particularly if your symptoms include sleep problems and/or depression. The ideal dose is 100mg, three times a day, or all three tablets one hour before sleep for sleep problems. Some practitioners recommend taking 5-HTP in combination with St John’s Wort (300 mg three times per day, 0.3 per cent hypericin content) and magnesium (200–250mg), also three times a day.
• Reduce your stress levels and learn how to relax. Stress management skills can help teach relaxation. Other relaxation methods, such as yoga, T’ai Chi and breathing exercises, can also be useful. Consider supplementing the herb Kava Kava as a muscle relaxant.
• Increase exercise slowly. Exercise should be gradually increased as the FM sufferer’s capacity for it increases. Posture and overall body structure need to be optimised, perhaps with the help of an osteopath or Alexander Technique teacher. Gentle massage, heat treatment and gentle stretching also help to improve muscle function and reduce pain.
• Also supplement: 2 x high potency multivitamin and mineral, 2 x vitamin CWhat it does: Strengthens immune system – fights infections. Makes collagen, keeping bones, skin and joints firm and strong. Antioxidant, detoxifying pollutants and protecting against… 1,000 mg, 2 x essential Omega 3 and 6 oil capsules, Magnesium Malate 600 mg (150 mg – 250 mg three times a day recommended in other sources), 5-HTP: 50-100 mg three times per day.
A growing number of people complain of moderate to severe muscle pain as they get older. As there may be no evidence of joint degeneration and inflammation, such problems are not classified as arthritis. Instead, they are often diagnosed as polymyalgia (pain in many places), fibromyalgia (pain in fibrous tissue) or fibrositis (inflammation of fibrous tissue). The differences between these can be confusing for both practitioner and patient; they are best distinguished by whether or not there is evidence of inflammation.
Fibrositis and Polymyalgia
Fibrositis is the name given to diffuse, rather than acute, muscle pain that responds to anti-inflammatory treatment, be it drugs or natural remedies.
It is highly likely to be the cumulative effect of either digestion and detoxification problems, poor blood sugar control, too many oxidants versus anti-oxidants, lack of essential fats, or allergies, or a combination of such factors which eventually programme the body for inflammatory reactions. In other words, it is likely to arise from an underlying imbalance in a person’s whole chemistry, so it is a case of tackling these causes rather than just suppressing the symptoms.
Polymyalgia rheumatica (PMR) is another group of symptoms that respond to anti-inflammatory treatment. Classic symptoms are pain (that does not ease with rest) in many areas of the body, often in the hands, wrists, feet and arms, such that a person is unable to raise their arms above shoulder height.
There is often a raised erythrocyte sedimentation rate (ESR) – a blood test which measures inflammation; and treatment frequently involves a course of steroid hormones such as prednisolone to relieve the pain. Again, this suggests a systemic problem where the body’s chemistry has gone into alarm mode, indicated by the state of inflammation. The symptoms will be eased by following the advice above.
REFERENCES
1. K. G. Henriksson and A. Bengtsson, ‘Fibromyalgia – a clinical entity?’ Canadian Journal of Physiology and Pharmacology, vol. 69 (5), 1991, pp. 672–7
2. A. Bengtsson and K. G. Henriksson, ‘The muscle in fibromyalgia – a review of Swedish studies’, Journal of Rheumatology, vol. 19 (suppl), 1989, pp. 144–9
3. J. Eisinger et al., ‘Glycolysis abnormalities in fibromyalgia’, Journal of the American College of Nutrition, vol. 13(2), 1994, pp. 144–8
4. M. Nicolodi and F. Sicuteri, ‘Fibromyalgia and migraine. Two faces of the same mechanism: serotonin as the common clue for pathogenesis and therapy’, Advances in Experimental Medicine and Biology, vol. 398, 1996, pp. 373–9; P. Sarzi Puttini and I. Caruso ‘Primary fibromyalgia syndrome and 5-hydroxytryptophan: a 90-day open study’, The Journal of International Medical Research, vol. 20 (2), 1992, pp. 182–9; See also K. Lawson, ‘Tricyclic antidepressants and fibromyalgia: what is the mechanism of action?’, Expert Opinion on Investigational Drugs, vol. 11 (10), 2002, pp. 1437-45
5. I. Caruso et al., ‘Double-blind study of 5-hydroxytryptophan versus placebo in the treatment of primary fibromyalgia syndrome’, The Journal of International Medical Research, vol. 18 (3), 1990, pp. 201–9
6. M. Nicolodi and F. Sicuteri, ‘Eosinophilia myalgia syndrome: The role of contaminants, the role of serotonergic set up’, Advances in Experimental Biology and Medicine, vol. 398, 1996, pp. 351–7
7. W. B. Weglicki et al., ‘Immunoregulation by neuropeptides in magnesium deficiency: ex vivo effect of enhanced substance P production on circulating T lymphocytes from magnesium-deficient mice’, Magnesium Research, vol. 9(1), 1996, pp. 3–11
8. M. S. Seelig, ‘Consequences of magnesium deficiency on the enhancement of stress reactions; preventive and therapeutic implications (a review)’, Journal of the American College of Nutrition, vol. 13(5), 1994, pp. 429–46
9. G. E. Abraham and J. Flechas, ‘Management of Fibromyalgia: Rational for the use of magnesium and malic acid’ Journal of Nutritional Medicine, vol. 3, 1992, pp. 49–59. V. Bobyleva-Guarriero and H. A. Lardy, ‘The role of malate in exercise-induced enhancement of mitochondrial respiration’, Archives of Biochemistry and Biophysics, vol. 245 (2), 1986, pp. 470–76
10. M. F. Holick, ‘Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis’, American Journal of Clinical Nutrition, vol. 79 (3), 2004, pp. 362-71
11. B. Regland et al, ‘Increased concentrations of homocysteine in the cerebrospinal fluid in patients with fibromyalgia and chronic fatigue syndrome’, Scandinavian Journal of Rheumatology, vol. 26 (4), 1997, pp. 301-7

Comments
Join the Conversation on our Facebook Page