The downside of cortisone creams
 The body’s own natural anti-inflammatory, released at times of emergency, is the adrenal hormone cortisolCortisol has been nicknamed ‘the stress hormone’ as it is released in higher levels during the body’s flight or fight response to stress. Levels of…. It is fat-based, originally derived from cholesterol, and is known as a steroid hormone. Cortisone-based cream that mimics cortisol, usually betnovate, is applied for eczema when the skin flares up. The creams may also contain anti-bacterial drugs.
The body’s own natural anti-inflammatory, released at times of emergency, is the adrenal hormone cortisolCortisol has been nicknamed ‘the stress hormone’ as it is released in higher levels during the body’s flight or fight response to stress. Levels of…. It is fat-based, originally derived from cholesterol, and is known as a steroid hormone. Cortisone-based cream that mimics cortisol, usually betnovate, is applied for eczema when the skin flares up. The creams may also contain anti-bacterial drugs.
Many eczema sufferers use this anti-inflammatory cream every day, as well as a moisturiser or emollient made out of petrolatum and hydrogenated vegetables oils to stop the skin from drying out and cracking.
Some hydrocortisone-based creams, such as Cortaid and Cortizone, can be bought over the counter. Higher-dose products that are generally available on prescription include triamcinolone (Aristocort, Kenalog), fluocinonide (Lidex), betamethasone (Valisone, Diprosone, Diprolene), mometasone (Elocon), and clobetasol (Temovate). In essence, they all work in the same way, by reducing inflammation.
They don’t have quite the same degree of danger as ingested cortisone, which gradually suppresses the body’s ability to makes its own, but they do have long-term side effects. Long-term use of cortisone creams isn’t desirable because they gradually damage the skin, making it thinner and more prone to drying and cracking. In fact, the changes in the collagen are identical to those seen in ageing. As a result the skin becomes more vulnerable to any infections and heals poorly. It’s a vicious cycle; the more you use the creams to help with the problems, the worse they become. Some of the preparations contain fluorine.
 Hidden Food Allergies
Hidden Food Allergies
This book will help if you feel you may be intolerant to a food, find it impossible to lose weight or simply have a range of minor symptoms your doctor can’t treat. Read More
Although possibly more effective, the fluorinated preparations such as Lidex are even more likely to cause skin thinning (particularly on the face, armpits, and groin), and they shouldn’t be used for prolonged periods on the face or around the eye. Higher-strength glucocorticoids, in particular, should be spread in a very thin layer, covering only the area requiring treatment. For most conditions, applying the medication once daily will suffice. (1) Of course, none of these creams do anything to address the underlying causes of the over-inflammation associated with eczema. And they have considerable long-term side effects.
Fortunately, there are natural solutions which, for some, can eliminate the need for medication completely and for most can reduce the need for medication.
Natural alternatives
In most cases the root cause of the inflammation is often a combination of exposure to irritants, unidentified allergies, and a predisposition to inflammatory reactions which can be activated by the wrong kind of diet, as well as stress and anxiety.By tackling the root causes, most people find partial to complete relief.
This means:
• Checking for airborne, food or chemical allergies
• Ensuring an optimum intake of anti-inflammatory nutrients
• Reducing the use of anti-inflammatory drugs
• Balancing blood sugar, reduce stress and the use of stimulants
• Healing the skin with antioxidant-based creams
The nutritional approach to eczema is based on the idea that a sufferer’s total environmental ‘load’ – that is, how much pollution, stress and poor nutrition they are dealing with – has exceeded their capacity to adapt to it. While there may be a specific trigger, such as an emotional crisis, drinking too much coffee or eating a food allergenAn allergen is a substance that is foreign to the body and which can cause an allergic reaction in certain people. Pollen is an example…, these can be seen as the final straw rather than the root cause. So the goal becomes to increase a person’s adaptive capacity and to lessen the total load. Anti-inflammatory drugs, by contrast, merely suppress symptoms.
Identifying hidden allergies
 Food allergies often develop when solid foods are introduced too early in the first six months of life. Ideally, a baby should be exclusively breast-fed for at least 4 months, ideally 6, and only introduced to high allergy-provoking foods such as cow’s milk, wheat and eggs, after 12 months. This is especially important if there is an inherited risk, with one or more parents suffering from allergy. (2)
Food allergies often develop when solid foods are introduced too early in the first six months of life. Ideally, a baby should be exclusively breast-fed for at least 4 months, ideally 6, and only introduced to high allergy-provoking foods such as cow’s milk, wheat and eggs, after 12 months. This is especially important if there is an inherited risk, with one or more parents suffering from allergy. (2)
The two main types of allergies, IgE and IgG, refer to different kinds of antibodies produced by your immune system. IgE or immunoglobulin E antibodies cause the more severe and immediate reactions. These are conventional allergies where, for example, a person’s skin flares up if they eat shellfish, or their breathing immediately constricts when they eat a peanut. People with allergies are often found to have higher levels of IgE, making them hypersensitive to certain substances. You can test your IgE sensitivity and identify specifically what you are reacting to from an IgE blood test. If you have eczema you may already have had this done. If not, ask your doctor or arrange it yourself. These tests are available direct to the public. However, most eczema suffers also have IgG-based allergies to foods. These are less obvious, and are sometimes called food intolerances or hidden allergies because they don’t cause immediate or severe reactions. Symptoms may not occur for a full 24 hours. Foods that commonly trigger IgG reactions are milk products, glutenGluten is a protein found in the cereals wheat, rye and barley. Obvious sources of gluten in the diet are bread, pasta, breakfast cereals and… cereals (wheat, rye, barley, oats), eggs and yeast. Your doctor is unlikely to offer an IgG allergy test, but you can test yourself using a home test kit (see www.yorktest.com for IgG food intoleranceFood intolerance is not the same as a food allergy. Food intolerances tend to cause digestive symptoms such as bloating, cramps and diarrhoea, but are… testing).
In a study involving 183 eczema sufferers who had the Yorktest Foodscan, and then avoided the identified foods, 83 per cent reported a moderate, high or considerable benefit to their eczema symptoms, with symptoms usually resolving in three weeks. (3) An example of improvement following removal of identified IgG intolerances is shown below. So, if you are tested and do have IgG sensitivities, and avoid them, there’s a good chance you’ll benefit.

BEFORE removal of food intolerances and AFTER removal of food intolerances The most common food allergyA food allergy occurs when the body’s immune system reacts abnormally to a specific food as it is perceived as a threat. In the most… that can provoke eczema, especially in children, is milk. IgG antibodies to milk have been found to be much more common in both children and adults with eczema. (4) (5) (6) (7) (8) Other researchers have also found IgG sensitivity to eggs to be far more common in eczema sufferers. (9)
But despite the overwhelming evidence of an association with a hidden IgG food allergy, very few eczema sufferers are tested for allergy by their doctors. Those that do are invariably tested for IgE-based reactions, yet these account for only a small fraction of food intolerances. If you have been tested, check which one it was and then have the other one done.
Case Studies
Liza is someone who benefited from finding the root cause of her eczematic reactions. She had used betnovate and other steroid-based creams all her life. After taking an IgG test, she found she was strongly allergic to dairy products and mildly sensitive to gluten and egg white. She was also taking in a lot of caffeine every day – several cups of coffee and a couple of Red Bull drinks. We advised her to take the allergens out of her diet for several months and to cut out the caffeine, which raises levels of the stress hormones adrenalin and cortisol. You might think that caffeine’s adrenal boost would reduce eczema, but substances that reliably indicate inflammation, such as interleukin-6, TNF, C-reactive proteinProteins are large molecules consisting of chains of amino acids. Proteins are essential nutrients for the human body – they are a building block of… and homocysteineHomocysteine is an amino acid found in the blood. Elevated levels of homocysteine have been associated with narrowing and hardening of the arteries, an increased… (10) are all raised by caffeine. A Greek study from 2004 that involved over 3,000 participants found that those consuming 200ml of coffee – two cups – had a 50 per cent higher level of interleukin-6, a 30 per cent higher C-reactive protein and a 28 per cent higher level of TNF compared to non-coffee consumers. (11)
I also recommended a vitamin A-based skin cream called Environ, which can help to keep the skin healthy once the inflammation calms down. One month later, Liza said: “I feel so much better. Nothing like as tired. I have one coffee a week, no headaches, no side effects. No bloating. The milk avoidance itself wasn’t so difficult. But I was amazed to find out how many foods had hidden milk, so it took a week to discover what I could and couldn’t have. Overall, it’s been fine. It’s not as hard as it used to be at the beginning. My skin is a lot better. I have no sores or cuts. The vitamin A cream really works very well.” Three months later, Liza was still eczema-free and did not have to use the betnovate cream once since she went on her allergy-free diet.
Amanda is another success story. She was diagnosed with eczema which developed following a kidney failure. She took her dermatologist’s advice and tried numerous products but with little success. “When my condition was bad, my hands and arms were red, painful and swollen. I couldn’t put my hands in water, I couldn’t bend my wrists or move my hands, I couldn’t cook or write. I work in administration and at times it was so bad that I had to take time off work. I tried everything from steroid creams and drugs to perfume and additive-free moisturisers. Nothing worked and even the simplest creams really stung my inflamed skin. Everything made it burn and go red and flaky.” she said. After suffering with her dry, flaky skin for three years, a therapist at her regular beauty salon suggested that she try applying Environ’s vitamin A and E body oil to one of her hands – a discovery that delighted her. “Vitamin A is supposed to be good for making skin function normally but after everything else I’d tried, I expected this to irritate my skin too. It was amazing, it didn’t sting and after a week the hand I tried it on was already looking better. My skin looked completely normal after I’d used the oil for three weeks.” Here’s what her hands looked like before and after the vitamin oils.

BEFORE and AFTER
Four years on Amanda reported that having continued using the Environ oil, supported by taking Omega 3 capsules, the dry skin she used to experience on her hands and arms had not returned. She only got the occasional redness that soon calmed.
 Hidden Food Allergies
Hidden Food Allergies
Hidden food allergies or intolerances can play havoc with your health, find out the best way to spot them. Read More
Antioxidants
It is known that inflamed tissue results in more oxidants, so it’s sensible to up your intake of antioxidants to counter the inflammation of eczema. Numerous studies have shown that a high intake of fresh fruit and vegetables – which boosts antioxidantAntioxidants are substances that protect cells within the body from damage caused by free radicals. They help to strengthen the body’s ability to fight infection… levels – reduces the severity of eczema.
Also, if a parent during pregnancy has higher intake of green and yellow vegetables, citrus fruit and beta-carotene in pregnancy this appears to reduce risk of their child developing eczema. (12)
Combating these conditions means eating lots of broccoli, peppers, berries, citrus fruit, apples (all rich in vitamin CWhat it does: Strengthens immune system – fights infections. Makes collagen, keeping bones, skin and joints firm and strong. Antioxidant, detoxifying pollutants and protecting against…), carrots and tomatoes (rich in beta-carotene and the powerful carotenoidCarotenoids are the colourful plant pigments that make fruits and vegetables orange, red and yellow in colour. They are powerful antioxidants. Examples of carotenoids include… lycopene) and seeds and fish (rich in vitamin A, E and seleniumWhat it does: Antioxidant properties help to protect against free radicals and carcinogens, reduces inflammation, stimulates immune system to fight infections, promotes a healthy heart,…). Vitamin C is a natural antihistamineAn antihistamine is a substance that prevents the action of histamine. Antihistamines are commonly used for the relief of allergic reactions such as hay fever…, enhancing the action of the enzyme histaminase, which quickly breaks down histamineHistamine is a chemical naturally produced by various cells in the body. A large amount of histamine is produced within mast cells where it forms… – the chemical that prompts inflammation during an allergic reaction. That means it will give you instant relief from an asthma attack or eczema flare-up, as long as you take enough.
One gram of vitamin C reduces blood histamine by approximately 20 per cent, and 2g reduces histamine by over 30 per cent. (13) There’s also evidence that people supplementing 1g of vitamin C a day are able to reduce their need for corticosteroids, and along with that their risk of negative side effects. (14) Another study has found that for every milligram of vitamin EWhat it does: Acts as an antioxidant, protecting cells from damage, including against cancer. Helps body use oxygen, preventing blood clots, thrombosis, atherosclerosis. Improves wound… in the diet, there is a drop in the level of IgE in the blood of asthma sufferers. (15) If the same is found to be true for eczema sufferers I would therefore recommend supplementing 200mg of vitamin E every day.
As far as supplements to optimise antioxidant intake are concerned, I would recommend taking a high-strength multivitamin and mineral, plus 1g of vitamin C with berry extracts (which are high in bioflavonoidsBioflavonoids are sometimes referred to as vitamin P. Flavonoids are widely distributed in plants and are known for their antioxidant activity….) and a good antioxidant formula that provides both vitamins A, C, E, zincWhat it does: Component of over 200 enzymes in the body, essential for growth, important for healing, controls hormones, aids ability to cope with stress…, selenium and glutathione and/or N-acetyl-cysteine (see below). The multivitamin also provides important B vitamins, which help reduce allergic potential. However, while all this makes good sense there is not convincing evidence that any (16) particular antioxidant supplement will make much of a difference on its own.
Switching to antioxidant creams.
Eczema sufferers may have a lot of skin damage caused by oxidants, so creams are important. Alternatives to the problematic cortisone creams are products containing the powerful antioxidant vitamins A, C and E. These have proven highly beneficial. (17)
There are also reports that vitamin DWhat it does: Helps maintain strong and healthy bones by retaining calcium. Deficiency Signs: Joint pain or stiffness, backache, tooth decay, muscle cramps, hair loss…., applied to the skin, can be very beneficial, (18) and at Toho University in Chiba, it was found that more than 80 per cent of patients with dry, inflamed eczematic skin responded favourably to home care treatment with vitamin-based skin creams. Another trial in patients with facial dermatitis resulted in major improvements, to the point where the people concerned could stop using cortisone creams. (19) The patients were asked to stop using topical steroids and to substitute a moisturising gel or cream containing vitamins A, C, E, beta-carotene and pro-vitamin B5 (panthenol), or an anti-oxidant gel containing tea tree oil. Topical vitamin A and C are the most potent skin healers. In cream form, vitamin A effectively treats the negative side effects of steroids, encouraging the skin to produce a better water-proofing barrier and significantly reducing the dry skin that arises with eczema.
The gentle retinyl palmitate form of vitamin A should be used rather than the acid form. By combining low-dose vitamin A and an antioxidant cream or gel, you can expect to see about an 80 per cent chance of significant improvement of the skin. It is important, though, to start with low levels, but not too low. If a skin cream provides less than 100iu (33mcg) of vitamin A per gram it’s not worth it. On the label you have to look for retinol palmitate or acetate or retinol. On rare occasions, starting with too high a concentration of vitamin A, for example double or triple this amount, can further aggravate the skin. Skin that has been treated with corticosteroids is severely malnourished, and ‘overfeeding’ with vitamins would add to the stress. So begin with small amounts of A and C cream on the skin plus the A you’ll get from a high-strength multivitamin, and gradually increase the amount. This is best done with the guidance of a skin care therapist used to applying vitamin A-based creams.
Natural anti-inflammatories
We’ve seen how the swelling of the airways, known as bronchioles, in asthma results from an inflammatory reaction. Steroid inhalers are anti-inflammatories, mimicking the action of the body’s own anti-inflammatory adrenal hormone, cortisol. Natural anti-inflammatories can be equally effective in reducing inflammation in the skin, including omega-3 fats, MSM, quercetin, zinc, magnesiumWhat it does: Strengthens bones and teeth, promotes healthy muscles by helping them to relax, also important for PMS, important for heart muscles and nervous…, ginger and turmeric.
The omega connection
Meat and dairy products are high in arachidonic acid, a type of omega-6 fatThere are many different types of fats; polyunsaturated, monounsaturated, hydrogenated, saturated and trans fat. The body requires good fats (polyunsaturated and monounsaturated) in order to… that can promote inflammation, while flax and chia seeds and oily fish are high in omega-3s.
These are anti-inflammatory. So too are a type of omega 6 fat, GLAGamma Linolenic Acid (GLA) is an essential fatty acid within the omega-6 family. It is found primarily in plant based oils such as evening primrose…, found in evening primrose and borage oil. A number of studies have found that supplementing evening primrose oil, a rich source of gamma-linolenic acid (GLA), the most potent omega 6 fat, reduced both the itching, redness and swelling in eczema, with benefits appearing after four to eight weeks. However, the benefit is less the more a person uses cortisone creams. (20) Increasing omega 3s may help too.
A study in Japan found that children who ate more omega 3 rich fish have less risk of eczema, (21) while another gave supplements during pregnancy and reported a lower incidence of eczema (22). Another gave infants with a high risk of developing eczema an omega 3 fish oil supplement during the first six months and found a lower risk of developing eczema, but this was not statistically significant. (23) I would certainly recommend a diet low in meat and dairy and high (that is, three times a week) in oily fish such as sardines, herrings and mackerel. It’s a good idea, too, to have a tablespoon of ground flax seeds or chia seeds and a daily supplement of 600mg of EPAEPA is short for Eicosapentaenoic Acid. It is an essential omega-3 fatty acid found in fish such as salmon, mackerel and herring, and is often…, 400mg of DHADHA is short for Docosahexaenoic Acid. It is an essential omega-3 fatty acid found in fish such as salmon, mackerel and herring, and is often… and 200mg of GLA each day, as the ideal balanced intake.
MSM – the magic molecule.
MSM (methylsulfonylmethane) is a non-toxic, natural component of the plants and animals we eat and is also found naturally in breast milk. This molecule contains a highly usable form of sulphur, the fourth most abundant mineral in the human body and part of the chemical makeup of over 150 compounds (all the proteins, as well as sulphur-containing amino acidsAmino acids are commonly known as the building blocks of protein. There are 20 standard amino acids from which almost all proteins are made. Nine…, antibodies, collagen, skin, nails, insulinInsulin is a hormone made by the pancreas. It is responsible for making the body’s cells absorb glucose (sugar) from the blood…., growth hormone and the most potent antioxidant, the enzyme glutathione). Vegans and people on a high-carbohydrate, low-protein diet probably don’t get enough MSM. Antibiotic overuse may also contribute to sulphur deficiency by killing off the intestinal bacteria needed to produce essential sulphur-containing amino acids. Correcting any MSM deficiency is important for eczema sufferers, as it’s particularly effective at damping down allergic responses to food and pollen.
MSM also provides the intestinal bacteria with building blocks for the manufacture of major anti-allergy, anti-inflammatory sulphur-containing amino acids, such as methionine and cysteine. Cysteine goes on to increase the production of glutathione, low levels of which are associated with inflammation. Onions and garlic are rich in cysteine. Along with vitamin C, cysteine is also needed for the production of collagen, the major component of connective tissue. Cysteine itself is very helpful in reducing asthmatic tendencies if supplemented at levels of 400mg or more. (24) MSM helps to bond collagen fibres together, giving elasticity to the skin; it is also very effective in helping the repair of damaged or scarred skin. I know of a number of anecdotal reports of recovery from eczema and there’s one published on ichtyosis, a genetic skin disorder characterised by dry, scaly and flaky skin, in which the application of MSM cream made a remarkable difference. (25)
The daily therapeutic dose for MSM ranges from 1,000 to 6,000mg – it can be that high because it’s as safe as drinking water. MSM works better if taken with vitamin C. Bear in mind that MSM is not like aspirin or a shot of cortisol. A single, one-time dose of it is rarely effective in lessening symptoms, so you’ll have to stick with it for a bit. A reduction in inflammation and other allergic symptoms is usually seen within two to 21 days. While all the supplement doses given here are for adults, if you have a child with eczema, the rule of thumb is to divide by body weight. So a 5 stone (about 32kg) child needs roughly half the amount, for example 500mg to 2,000mg.
Quercetin – bioflavonoid boon.
The bioflavonoids are a group of 4,000 antioxidant and anti-inflammatory chemicals that are found in many plants and have a range of therapeutic effects. Quercetin is one that many nutritional therapists swear by for allergies, reporting that a once-a-day supplement can often reduce allergic symptoms across the board. There have not yet been any double-blind trials of quercetin’s benefits, but there is evidence that quercetin can reduce the activity of mast cells – the ones that release the inflammatory chemicals such as histamine, certain prostaglandins, and the inflammatory ‘messengers’ leukotrienes. (26) That would account for its value in treating allergies. Quercetin is naturally found in wine, but not beer; tea, but not coffee; and the outer layers of red and yellow onions, but not white onions (see ‘Quercetin-rich foods’). For the best effect, you’ll need to supplement it, ideally in combination with vitamin C and a high-potency bromelain (the enzyme found in pineapple). For most people, the effective therapeutic dose is 500mg of quercetin in combination with approximately 125mg of bromelain and 250 to 500mg vitamin C, taken 30 minutes before meals two to three times a day. For maintenance (after your allergic symptoms have been brought under good control), reduce the above dose to once or twice daily, 30 minutes before breakfast and/or again before dinner. Quercetin-rich foods 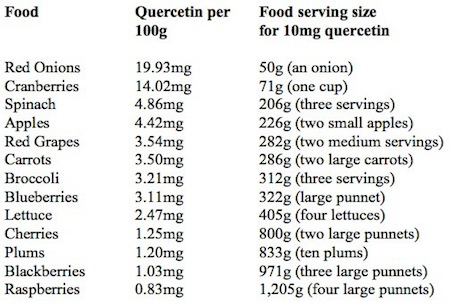
Zinc and magnesium – master minerals.
Magnesium is the second most abundant mineral in the human body. It works closely with calciumWhat it does: Promotes a healthy heart, clots blood, promotes healthy nerves, contracts muscles, improves skin, bone and dental health, relieves aching muscles and bones,… and vitamin B6 to regulate the heart, muscles, brain and immune system. It’s also needed for essential fats to work properly, and plays a significant role in the prevention and treatment of various allergy-related conditions, including eczema. One study from 1980 found that magnesium deficiency produced allergy symptoms in rats. (27)
If you’re not getting enough magnesium, you may experience symptoms such as constipation, cramps, headaches, insomnia and depression. We recommend eating plenty of green leafy vegetables, nuts, beans, lentils and seeds – especially pumpkin seeds. A small handful of pumpkin seeds (25g) will give you 150mg of magnesium. If you are also supplementing a high-strength multivitamin, that can provide a further 150mg. If you have asthma attacks quite frequently, it’s probably worth supplementing an additional 200mg of elemental magnesium in an easily absorbable form (such as magnesium glycinate, citrate or ascorbate) twice daily.
Zinc is another potential star in allergy treatments, turning out to be far more influential in the treatment of food allergy than anyone thought. The mineral is vital for making the essential fatty acidsEssential Fatty Acids (EFAs) are fats that must be taken in through the diet as they cannot be made by the body. Both omega-3 and… that are known to reduce inflammation, and it is also one of the most important nutrients for the immune system. (28) In animals, zinc deficiency makes the airway constrict, while giving zinc dilates them. (29) It’s needed for restoring the delicate linings of the airways and healing the skin. Although zinc on its own certainly isn’t a miracle cure, ensuring an optimal intake of zinc is likely to help both asthma and eczema. Although the RDA for zinc is 15mg per day, doses of 20 to 40mg have had beneficial effects in conditions common among food allergy sufferers, such as acne, dermatitis herpetiformis (an extremely itchy rash associated with coeliac disease), eczema, psoriasis, hyperactivity, eating disorders and learning disabilities. Daily doses of 40mg or higher should not be continued for longer than three months. Zinc also depletes the body of copper, so supplement 1mg of copper with every 10 to 15mg of zinc.
The spice route – ginger and turmeric.
 Ginger and the yellow curry spice turmeric have long been known to help inflammatory diseases. But exactly why they work has only recently been discovered.
Ginger and the yellow curry spice turmeric have long been known to help inflammatory diseases. But exactly why they work has only recently been discovered.
In inflammatory diseases, an inflammation-promoting protein known as nuclear transcription factor kappa B is produced. Ginger and turmeric, along with garlic and pepper, turn it off, thereby reducing inflammation. (30) That’s the reasoning behind the seasoning. While we await human trials, animal studies show that curcumin, which is the active ingredient in turmeric, has proven highly effective in reducing asthma symptoms. (31) No studies have yet been published on eczema. So I recommend the liberal use of both ginger and turmeric, or taking concentrated supplements, if you suffer from either eczema or asthma. Luckily, they’re both tasty additions to curry and relishes in dried form, while fresh ginger is delicious grated with red lentils or sliced in stir-fries.
In summary
There’s little doubt that the main anti-inflammatory drugs used to treat eczema, while highly effective in providing relief, particularly in the short term, can make matters worse in the long run and incur risks for a variety of side effects. It’s equally obvious that checking for allergies, upping your intake of antioxidants, essential fats and other natural anti-inflammatories, improving your breathing if you have asthma, and applying appropriate vitamin-based skin creams if you have eczema constitute an approach that at worst, is likely to reduce the need for drugs and at best, will completely relieve symptoms. While there’s a lack of good studies to prove the benefits of an all-round nutrition-based approach, there’s certainly every good reason to pursue these and see what happens to your symptoms. What works:
• Eat a diet high in oily fish (wild or organic salmon, mackerel, herring, kippers, sardines and tuna steak a maximum of once a week), omega-3 rich flax and pumpkin seeds, and low in meat and milk. Also supplement 1,000mg of the combined omega-3s EPA/DHA, which usually means two to three fish oil capsules a day.
• Check yourself for food allergies with a proper food allergy test (see www.yorktest.com).
• Supplement 1,000 to 2,000 mg of MSM and 400mg or more of N-acetyl-cysteine.
• Include plenty of organic free-range eggs (the omega-3-rich type are excellent too), red onions and garlic in your diet, all high in sulphur.
• Eat plenty of fruit and vegetables high in antioxidants.
• Add ginger and turmeric to your food.
• Take a good all-round multivitamin with at least 1,000mg of vitamin C, 150mg of magnesium and 10mg of zinc.
• Supplement an all-round antioxidant formula if you don’t eat at least six servings of fruit and vegetables a day, although eating plenty of them is very important. Also supplement 1,000mg of quercetin a day.
• If you have asthma, learn how to breathe using the Buteyko method.
• For eczema, apply vitamin A and C skin creams daily.
Dig deeper by reading my book, co-authored with Natalie Savona, Solve Your Skin Problems. The book Hidden Food Allergies also can be helpful in understanding causes of eczema..
Visit HOLFORDirect.com – home of GL friendly foods, supplements, tests and books.
Working with your doctor
Many of the recommendations made here to reduce your inflammatory and allergic sensitivity can be put into action without interfering in any way with medical treatment. And they may well reduce the need for it. For instance, if you have eczema and find that some of the measures we’ve outlined here are making your skin much less dry, inflamed and sore, you may find that your need for cortisone-based creams becomes less. One of the most important factors to check for is allergy. Your doctor may be willing to refer you for allergy tests. It is important, however, that you are checked for both IgE and IgG allergies, so as few doctors check for IgG-based allergies, you may need to do it using a home test kit (see www.yorktest.com).
REFERENCES
1. Topical steroids for atopic dermatitis in primary care. Drug and Therapeutics Bulletin, Jan 2003; 41: 5 – 8.
2. Szajewska H. Early nutritional strategies for preventing allergic disease. Isr Med Assoc J. 2012 Jan;14(1):58-62. Review.
3. G.Hardman, G.Hart, Dietary advice based on food-specific IgG results, Nutrition & Food Science, 2007, Vol. 37 Iss: 1, pp.16 – 23
4. Firer, M A et al., Cow’s milk allergy and eczema: Patterns of the antibodyAn antibody is a protein produced by the body’s immune system when it detects a harmful substance known as an antigen. Examples of antigens include… response to cow’s milk in allergic skin disease, Clin Allergy, vol 12, pp 385-90 (1982)
5. Shakib, F et al., Relevance of milk- and egg-specific IgG4 in atopic eczema, Int Arch Allergy Appl Immunol, vol 75, pp 107-12 (1984) and Shakib F et al., Study of IgG sub-class antibodies in patients with milk intolerance, Clin Allergy, vol 16, pp 451-8 (1986)
6. Husby, S, et al., IgG subclass antibodies to dietary antigens in atopic dermatitis, Acta Derm Venereol Suppl, vol 144, pp 88-92 (1989)
7. Iikura, Y et al., How to prevent allergic disease I. Study of specific IgE, IgG, and IgG4 antibodies in serum of pregnant mothers, cord blood, and infants, Int Arch Allergy Appl Immunol, vol 88, pp 250-2 (1989)
8. Lucarelli, S et al., Specific IgG and IgA antibodies and related subclasses in the diagnosis of gastrointestinal disorders or atopic dermatitis due to cow’s milk and egg, Int J Immunopathol Pharmacol, vol 11, pp 77-85 (1998)
9. Niggemann, B et al., Outcome of double-blind, placebo-controlled food challenge tests in 107 children with atopic dermatitis, Clin Exp Allergy, vol 29, pp 91-96 (1999)
10. D Panagiotakos et al ‘The association between coffee consumption and plasma total homocysteine levels:the ‘ATTICA study’ Heart Vessels, vol 19(6), pp. 280-6 (2004)
11. A. Zampelas et al., Associations between coffee consumption and inflammatory markers in healthy persons: the ‘ATTICA study’, American Journal of Clinical Nutrition, Vol. 80(4), pp. 862-867 (2004)
12. Miyake Y et al., Consumption of vegetables, fruit, and antioxidants during pregnancy and wheeze and eczema in infants. Allergy. 2010 Jun 1;65(6):758-65. Epub 2010 Jan 22
13. A. Soutar, Bronchial reactivity and dietary antioxidants, Thorax, vol 52, pp 166-170 (1997)
14. A. Fogarty et al., Corticosteroid sparing effects of vitamin C and magnesium in asthma: a randomised trial, Respir Med, vol 100(1), pp. 174-9 (2006)
15. A. Fogarty et al., Dietary vitamin E, IgE Concentrations,and Atopy’, The Lancet, vol 356 (9241), 2000, p.449-52
16. Bath-Hextall FJ et al., Dietary supplements for established atopic eczema. Cochrane Database Syst Rev. 2012 Feb 15;2:CD005205. Review
17. G. Panin et al., Topical alpha-tocopherol acetate in the bulk phase: eight years of experience in skin treatment, Ann N Y Acad Sci, vol 1031, pp. 443-7 (2004) Review
18. K. Egawa, Topical vitamin D3 derivatives in treating hyperkeratotic palmoplantar eczema: a report of five patients.J Dermatol. 2005 May;32(5):381-6
19. E. Tanabe, Treatment of intractable facial lesions of adult atpoic dermatitis with Environ mild night cream’ Aesthetic Dermatology, vol 5, p.1119-122, (1995)
20. Morse NL, Clough PM. A meta-analysis of randomized, placebo-controlled clinical trials of Efamol evening primrose oil in atopic eczema. Where do we go from here in light of more recent discoveries? Curr Pharm Biotechnol. 2006 Dec;7(6):503-24. Review.
21. Kunitsugu I et al., ‘Self-reported seafood intake and atopy in Japanese school-aged children.’ Pediatr Int. 2012 Apr;54(2):233-7
22. Palmer DJ et al ‘Effect of n-3 long chain polyunsaturated fatty acid supplementation in pregnancy on infants’ allergies in first year of life: randomised controlled trial.’ British Medical Journal. 2012 Jan 30;344:e184.
23. D’Vaz N et al., ‘Postnatal fish oil supplementation in high-risk infants to prevent allergy: randomized controlled trial.’ Pediatrics. 2012 Oct;130(4):674-82.
24. E Grandjean et al, Efficacy of oral long-term N-acetylcysteine in chronic bronchopulmonary disease: a meta-analysis of published double-blind placebo-contrlled clinical trials, Clinical Therapuetics, vol 22(2), pp. 209-221 (2000)
25. C.A. Fleck, Managing ichthyosis: a case study. Ostomy Wound Manage, 2006 Apr;52(4):82-6
26. E. Middelton and G. Drzewiecki, Effects of flavanoids and transitional metal cations on antigern-induced histamine relase from human basiphils, Biochem Pharmacolo, vol 31(7), pp. 1449-53 (1982) and E. Middelton and G. Drzewiecki,, Flavoindi inhibition of human basohpil histamine release stimulated by various agents, Biochem Pharmacolo, vol 33(21) pp. 3333-8 (1984)
27. S. Claverie-Benureau , Magnesium deficiency allergy-like crisis in hairless rats: a suggested model for inflammation studies, J Physiol (Paris), vol 76(2), pp. 173-5 (1980)
28. J. E. Sprietsma, Modern diets and diseases: NO-zinc balance. Under Th1, zinc and nitrogen monoxide (NO) collectively protect against viruses, AIDS, autoimmunity, diabetes, allergies, asthma, infectious diseases, atherosclerosis and cancer, Med Hypotheses, vol 53, pp 6-16 (1999)
29. M. Richter et al., Zinc status modulates bronchopulmonary eosinophil infiltration in a murine model of allergic inflammation, Chest, vol 123(3 Suppl), pp. 446S (2003)
30. B. B. Aggarwal and S. Shishodia, Suppression of the nuclear factor-kappaB activation pathway by spice-derived phytochemicals: reasoning for seasoning, Ann N Y Acad Sci, vol 1030, pp. 434-41 (2004) Review
31. A. Ram et al., Curcumin attenuates allergen-induced airway hyperresponsiveness in sensitized guinea pigs, Biol Pharm Bull, vol 26(7), pp. 1021-4 (2003)

Comments
Join the Conversation on our Facebook Page