Anorexia – essentially, self-starvation – was first identified by Dr William Gull in 1874. This is his treatment: ‘The patient should be fed at regular intervals, and surrounded by persons who could have moral control over them, relations and friends being generally the worst attendants.’ Today, treatment is often essentially the same, summed up as ‘drug them, feed them and let them get on with their lives’ in an article in the Guardian describing treatment in ‘leading hospitals’. The ‘modern’ approach includes ‘behaviour therapy’, that is, rewards and privileges, and drugs to induce compliance. The drugs include psychotropic drugs such as chlorpromazine, sedatives and antidepressants. The diet is high carbohydrateCarbohydrates are the primary source of energy for the body as they can be broken down into glucose (sugar) more readily than either protein or…, sometimes as much as 5,000kcals, with little regard to quality.
Bulimia is binge eating followed by self-induced vomiting or laxative use, and is probably a more common condition nowadays – although it may also be the easiest to hide, as bulimics may approach or exceed normal weight. Some anorexics are also bulimic. Some bulimics are not anorexic. It is still a food/weight compulsive/obsessive disorder, characterised by:
• Recurrent episodes of binge eating (rapid consumption of large amounts of food in a discrete period of time)
• A feeling of lack of control over eating behaviour during the binges
• The person regularly engages in self-induced vomiting, use of laxatives, diuretics, strict dieting, fasting, or exercise in order to prevent weight gain.
• A minimum average of two binge eating sessions a week.
• Persistent over-concern with body shape and weight.
The ZincWhat it does: Component of over 200 enzymes in the body, essential for growth, important for healing, controls hormones, aids ability to cope with stress… Link
The idea that nutrition, or malnutrition, could play a part in the development and treatment of this condition did not really emerge until the 1980s, when scientists began to realise just how similar the symptoms and risk factors of anorexia and zinc deficiency were (see table below). As early as 1973 two zinc researchers, K. Hambidge and A. Silverman, concluded that ‘whenever there is appetite loss in children zinc deficiency should be suspected’ [1]. In 1979, Rita Bakan, a Canadian health researcher, noticed that the symptoms of anorexia and zinc deficiency were similar in a number of respects and proposed that clinical trials be undertaken to test its effectiveness in treatment [2]. Meanwhile, David Horrobin, most renowned for his research into evening primrose oil, proposed that ‘anorexia nervosa is due to a combined deficiency of zinc and EFAs’ [3].
More recently, strong evidence has come to light that those with anorexia and bulimia may be more prone to tryptophan deficiency. Tryptophan is the building block for serotoninSerotonin is a hormone found naturally in the brain and digestive tract. It is often referred to as the ‘happy hormone’ as it influences mood…., the brain’s ‘happy’ neurotransmitterA neurotransmitter is a chemical messenger that carries signals between body cells. They are various types of neurotransmitters which play a major role in everyday…, that also helps control appetite. 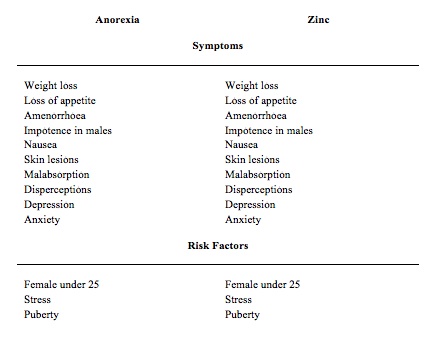 Zinc Hypothesis Confirmed In 1980, when the zinc link had been reported, the first trial started at the University of Kentucky. The researchers discovered that 10 out of 13 patients admitted with anorexia and 8 out of 14 patients with bulimia were zinc deficient on admission. After vigorous feeding they became even more zinc deficient. Since zinc is required to digest and utilise proteinProteins are large molecules consisting of chains of amino acids. Proteins are essential nutrients for the human body – they are a building block of…, from which body tissue is made, they recommended that extra zinc, above that required to correct deficiency, should be given as the anorexic starts to eat and gain weight [4]. In 1984 the penny dropped with two important research findings and the first case of an anorexic treated with zinc.
Zinc Hypothesis Confirmed In 1980, when the zinc link had been reported, the first trial started at the University of Kentucky. The researchers discovered that 10 out of 13 patients admitted with anorexia and 8 out of 14 patients with bulimia were zinc deficient on admission. After vigorous feeding they became even more zinc deficient. Since zinc is required to digest and utilise proteinProteins are large molecules consisting of chains of amino acids. Proteins are essential nutrients for the human body – they are a building block of…, from which body tissue is made, they recommended that extra zinc, above that required to correct deficiency, should be given as the anorexic starts to eat and gain weight [4]. In 1984 the penny dropped with two important research findings and the first case of an anorexic treated with zinc.
The first study, since confirmed, showed that animals deprived of zinc very rapidly developed anorexic behaviour and loss of appetite, and that if these animals were force-fed a zinc-deficient diet to gain weight, they became seriously ill [5]. The second study showed that zinc deficiency damages the intestinal wall and therefore the absorption of nutrients including zinc, potentially leading to a vicious spiral of deficiency [6]. Then, in 1984, Professor Derek Bryce-Smith, now patron of the Institute for Optimum Nutrition, reported the first case of anorexia treated with zinc. The patient was a 13-year-old girl, tearful and depressed, weighing 37kg. She was referred to a consultant psychiatrist, but, despite counselling, three months later her weight was 31.5kg (under 5 stone). Within two months of zinc supplementation at a level of 45mg per day, her weight returned to 44.5kg, she was cheerful again, and tests for zinc deficiency were normal [7].
Meanwhile, the first double-blind trial with 15 anorexics was being carried out at the University of California. In 1987 the researchers reported: ‘Zinc supplementation was followed by a decrease in depression and anxiety. Our data suggest that individuals with anorexia nervosa may be at risk for zinc deficiency and may respond favourably after zinc supplementation.’[8] By 1990, many researchers had found that over half of anorexic patients showed clear biochemical evidence of zinc deficiency [9]. In 1994 Dr Carl Birmingham and colleagues carried out a double-blind controlled trial giving 100mg of zinc gluconate or a placebo to 35 women with anorexia. They concluded that ‘the rate of increase in body mass of the zinc supplemented group was twice that of the placebo group and this difference was statistically significant’ [10].
Sadly, many treatment centres still fail to supplement those suffering from anorexia with zinc. Zinc: The Chicken or the Egg? The evidence linking zinc and anorexia is now beyond question. In fact, a recent review of all the research concludes: ‘There is evidence that suggests zinc deficiency may be intimately involved with anorexia in humans: if not as an initiating cause, then as an accelerating or exacerbating factor that may deepen the pathology of anorexia.’ [11] The fact that high levels of zinc supplementation help to treat anorexia does not mean the cause of anorexia is zinc deficiency. Psychological issues may, and probably do, bring about change in the eating habits of susceptible people. By avoiding eating, a young girl can repress the signs of growing up. Menstruation stops, breast size decreases and the body stays small.
Starvation induces a kind of ‘high’ by stimulating changes in important brain chemicals, that may help to block out difficult feelings and issues that are too hard to face. Many anorexics also choose to become vegetarian, and most vegetarian diets are lower in zinc, essential fats and protein, according to a study at the Health Sciences Department of the British Columbia Institute of Technology in Burnaby, Canada, which analysed the diets of vegetarian anorexics, versus non-vegetarian patients.[12] Whether vegetarian or not, once the route of not eating is chosen and becomes established, zinc deficiency is almost inevitable, both due to poor intake and poor absorption. With it comes a further loss of appetite and even more depression, disperceptions, and the inability to cope with the stresses that face many adolescents, especially girls, growing up in the 21st century.
The optimum nutrition approach to help someone with anorexia, or bulimia, is best carried alongside work with a skilled psychotherapist. The nutritional approach emphasises quality of food rather than quantity, including supplements to ensure vitamin and mineral sufficiency, and of course 45mg of elemental zinc per day, halving this level once weight gain is achieved and maintained. Low Tryptophan: the Appetite Controller Loss of weight and loss of muscle tissue is an indication of protein deficiency. This can be the result of either insufficient intake, or inadequate digestion, absorption or metabolismMetabolism is a term that is used to describe the chemical reactions that take place within the body’s cells. The body gets the energy it…. The amino acidsAmino acids are commonly known as the building blocks of protein. There are 20 standard amino acids from which almost all proteins are made. Nine… valine, isoleucine and tryptophan have been found to be low in people with anorexia. Supplementing valine and isoleucine helps to build muscle, while tryptophan is the building block of serotonin, a neurotransmitter that controls both mood and appetite.
Recent research has found striking differences in blood levels of tryptophan in anorexic patients.[13] Also, both starvation and excessive exercise have been shown to influence the availability of tryptophan in the blood of anorexic patients.[14] To date, the evidence is pointing towards a problem with how people with eating disorders respond to low tryptophan. In fact, the conversion of tryptophan into serotonin is both zinc and B6 dependent. These three nutrients may all be needed for proper appetite control, as well as a balanced, happy mood. The interplay between body and mind, or nutrients and behaviour, is well illustrated by recent research at Oxford University’s psychiatry department by Dr Philip Cowen and colleagues which found, not surprisingly, that women on calorie-restricted diets develop lower levels of tryptophan and serotonin. However, recovered bulimics, when put on a diet free of tryptophan, rapidly become more depressed and overly concerned about their weight and shape, as well as more fearful of their loss of control over their eating.[15]
In a similar trial that deprived both women with bulimia and healthy ‘controls’ of tryptophan for one day, the bulimic women became more depressed and had a much greater desire to binge than the controls.[16] All this research strongly suggests that those prone to anorexia or bulimia have a special need for tryptophan, and probably zinc and B6, and that when deprived of these nutrients they are more likely to develop unhealthy reactions, including loss of appetite control. While supplementing tryptophan, or 5-hydroxytryptophan (5-HTP), plus zinc and B6, is the most direct way to address these imbalances in people with eating disorders, in the long run the goal must be to change the diet. Often, especially in those with anorexia, supplements, including concentrated fish oils, are more acceptable at first because unlike food they contain virtually no calories. However, as a person’s nutrition improves, so their anxieties and compulsiveness become better and they can see the logic for making dietary changes.
The ideal diet should include easily assimilable foods containing good-quality protein such as quinoa, fish, soya and spirulina or blue-green algae. Other good foods are ground seeds, lentils, beans, plus fruits and vegetables. Fish and seeds are especially important because they contain essential fats. Since most people with eating disorders go out of their way to avoid fatThere are many different types of fats; polyunsaturated, monounsaturated, hydrogenated, saturated and trans fat. The body requires good fats (polyunsaturated and monounsaturated) in order to…, their diets are frequently low in these essential nutrients. Also, essential fats are vital for the body to both make serotonin and to receive the serotonin signals that cross between one neuron and another. The optimum nutrition approach, therefore, involves ensuring all these nutrients are provided in optimal amounts. What’s Your Binge Food? In the case of bulimia, what a person binges on is very revealing, either of food sensitivities or blood sugar problems.
The most common binge foods are sweet foods, wheat foods or dairy foods. Both wheat and dairy products contain exorphins, chemicals that mimic (and can therefore block) pleasure-giving endorphins in the brain, and again, may influence behaviour. Sweetened foods, of course, satisfy a low blood sugar condition, and the cure is to eat foods that keep your blood sugar level even. I have often asked people with bulimia to binge as much as they like for the next two weeks, but not on these foods. Often they report that their desire to binge at all is dramatically reduced. Once again, these foods, in certain people, may provoke a change in mood and behaviour that sets them off on a slippery slope. Don’t think, however, that if a person is deficient, or has a biochemical uniqueness that makes them more prone to react strongly to the lack of a nutrient like zinc or tryptophan, that this excludes psychological problems as part of ‘the cause’.
Many people with anorexia are the bearers of a secret, a trauma or a problem that needs to be resolved, and can be with the help and support of a psychotherapist. A good place to start is contacting beat (formerly the Eating Disorders Association).
In summary, I recommend the following for anyone who is dealing with an eating disorder:
• See a clinical nutritionist who can assess what you are deficient in and advise you accordingly
• Their advice will probably include 30 to 50mg of zinc, 100mg of B6, 200mg of 5-HTP, plus essential fats, either in capsules or in seeds and fish
• See a psychotherapist with experience of helping people with eating disorders making a full recovery
REFERENCES
1. B. Gesch, SCASO pilot study data, unpublished
2. S.J.Schoenthaler, The Norther California diet-behaviour program: An Empirical evaluation of 3,000 incarcerated juveniles in Stanislaus County Juvenile Hall. Int J biosocial Res, Vol 5(2), 1983, pp. 99-106 and features on www.mentalhealthproject.com
3. B. Gesch, ‘Influence of supplementary vitamins, minerals and essential fatty acidsEssential Fatty Acids (EFAs) are fats that must be taken in through the diet as they cannot be made by the body. Both omega-3 and… on the antisocial behaviours of young adult prisoners’, Brit J Psychiatry, Vol 181, 2002, pp. 22-8
4. E. Noble, ‘The gene that rewards alcoholism’, Scientific American, Science and Medicine, March
5. U.D. Register et al., ‘The junk food connection – alcohol’, J Am Diet Assoc, Vol 61(2), 1972, pp. 159-62
6. A. F Libby et al., ‘The junk food connection – alcohol and drug lifestyle adversely affect metabolism and behaviour’, Orthomolecular psychiatry, Vol 11(2), 1982, pp. 116-27
7. Personal communication with Dr Abram Hoffer. See also W.E. Beebe and O.W. Wendel, Preliminary Observations of Altered Carbohydrate Metabolism in Psychiatric Patients, D. Hawkins and L. Pauling (eds), W.H. Freeman and Co. (1973), pp. 435-51
8. U.D. Register et al., ‘Influence of nutrients in intake of alcohol’, 1972
9. W. Philpott and D. Kalita, Brain Allergies, Keats Publishing (1980)
10. Society for the Study of Addiction. See www.addiction-ssa.org/
11. M.R. Werbach, Nutritional Influences on Mental Illness, Third Line Press (1991)
12.B. Spittle and J. Parker, ‘Wernicke’s encephalopathy complicating scizophrenia’, Aust and NZ J Psych, Vol 27, 1993, pp. 638-52
13. K. Eriksson et al., ‘Effects of thiamine deprivation and antagonism on voluntary ethanol intake in rats’, J Nutr, Vol 110, 1980, p.937
14. L.L. Rogers et al., ‘Voluntary alcohol consumption by rats following administration of glutamine’, J Biol Chem, Vol 220910, 1956, pp. 321-3
15. H. Ikeda, ‘Effects of taurine on alcohol withdrawal’, Lancet, Sept. 1977, Vol. 2(8036), p. 509
16. R.M. Guenther, ‘Role of nutritional therapy in alcoholism treatment’, Int J Biosoical Res, Vol 4(1), 1983, pp. 5-18

Comments
Join the Conversation on our Facebook Page