With 50 million people in the world diagnosed with dementia, two thirds of which develop Alzheimer’s dementia, with rapid brain shrinkage, hopes are high. But the sad truth is that each of these statements is a lie. Aducanumab, made by Biogen, is one of a number of drugs that target amyloid proteinProteins are large molecules consisting of chains of amino acids. Proteins are essential nutrients for the human body – they are a building block of… in the erroneous belief that the cause of Alzheimer’s is a build up of amyloid ‘plaque’ and blocking its formation could halt the progression. Every single one of this class of drugs has failed – including Aducanumab.
Another amyloid drug called Solanezumab had a brief moment of fame when a trial showed a 2 per cent reduction on brain shrinkage and tiny changes in cognitive tests but failed to produce any meaningful clinical dementia benefits.
In March 2019 Biogen announced they were halting their Phase 3 clinical trial of Aducanumab (ADU) due to futility – no benefit. The New York Times reported “An Alzheimer’s Treatment fails: we don’t have anything now. More than 300 failed trials. With high hopes, drugs to fight brain plaques were tested in people genetically destined to develop dementia. The drugs failed.”
In a normal world, if you test a theory 300 times and it fails 300 times you discard the theory – that amyloid plaques in the brain are what causes Alzheimer’s. I believe this theory, in which big pharma has invested tens of billions of dollars in research, is a red herring.
So why these recent headlines? Well, Biogen re-jigged their trial results and are claiming that a small subset of people in one of their trials could have got a little bit of benefit. They’ve resubmitted to the FDA, in the hope of getting their drug approved but will they?
“I doubt FDA will approve it. They are over optimistic.” says Emeritus Professor of Pharmacology David Smith from the University of Oxford. A critique by three eminent experts in Alzheimer’s – clinical neurologist Dr Davis Knopman from the Department of Neurology at the Mayo Clinic, Dr Michael Greicius from the Department of Neurology and Neurological Sciences at Stanford University’s School of Medicine, and radiologist Dr David Jones, reached the same conclusion. “The two ADU trials have raised many questions. While it is possible that ADU has cognitive benefits, the data as they exist are clearly insufficient to support a claim of efficacy. The finding of one positive and one negative result is a statement of inconclusiveness.”1
The reason I state that the media reports are a lie is that better and undisputed results have already been shown in trials giving B vitamins to those with high homocysteineHomocysteine is an amino acid found in the blood. Elevated levels of homocysteine have been associated with narrowing and hardening of the arteries, an increased… levels who have good omega-3 fatThere are many different types of fats; polyunsaturated, monounsaturated, hydrogenated, saturated and trans fat. The body requires good fats (polyunsaturated and monounsaturated) in order to… status. So, even if ADU did work, which has not been shown, it would certainly not be the ‘first drug to halt Alzheimer’s’.
Dementia Drugs versus Nutrients
Before reminding you of these results it’s worth knowing what researchers are looking for in successful clinical trials. Alzheimer’s, which accounts for two thirds of dementia, is diagnosed in two ways: firstly by a progressive loss of cognitive functions including memory, language, judgement, praxis and orientation and secondly, by a specific kind of brain scan of a central area of the brain called the ‘medial temporal lobe’.
While this type of brain scan, developed by Professor David Smith’s team at Oxford University is used worldwide for diagnosis, most studies use a simpler type of scan of the whole brain, reporting changes in the rate of brain shrinkage. ADU has not published any changes in brain shrinkage. Solanezumab, another amyloid targeting drug, showed a non-significant 2% reduction in brain shrinkage. In contrast, the combination of B vitamins and sufficient omega-3 has shown a highly significant 68% less brain shrinkage over a year. No other drugs or treatments have shown such a large positive effect on the rate of brain shrinkage.
The other hallmark of potential benefit is to measure a ‘biomarker’ or risk factor for Alzheimer’s and see if the treatment improves these and that these improvements in the biomarker track positive changes in clinical symptoms and measures of cognitive function. The biomarker used in the ADU trial is amyloid protein while the one I like and predicts Alzheimer’s risk better is blood level of ‘homocysteine’. Approximately 40% per cent of those over 70 and two in three diagnosed with memory problems have raised homocysteine at levels associated with increased brain shrinkage (above 11µmol/l).
The ADU drug trial found changes in measures of amyloid protein but these changes didn’t track with cognitive changes. And there lies a problem – if you pick a marker, change it with a drug, but it doesn’t change actual symptoms, then the marker should be considered redundant. A recent meta-analysis of 14 anti-amyloid clinical trials on 4,596 patients found no slowing of cognitive decline in spite of significant lowering of brain amyloid.2 But, with so much invested in the amyloid story big pharma are resisting moving on.
In contrast, in the B vitamin trials homocysteine levels fall in line with improvement in cognitive function as I’ll show below. Two major studies of studies, one by researchers at the National Institutes of Health in the US3 analysing 247 trials and the other by Professor Jin-Tai Yu from Shanghai’s Yudon University, who examined 396 trials, concluded that raised homocysteine, easily lowered by B vitamins, was the most predictive marker and disease-modifying treatment, accounting for a quarter of the risk for Alzheimer’s.
The ultimate measure of improvement are changes in cognitive function since that is, after all, what a person with Alzheimer’s suffers from. This can be measured in two ways: by running specific cognitive function tests of the ‘skills’ that decline in Alzheimer’s namely verbal or visuospatial memory recall, processing speed, attention and executive function tasks requiring planning or judgement & semantic fluency; and by changes in the clinical dementia rating which is what a psychiatrist would use to assess improvement.
Both ADU and Solanezumab showed insignificantly small improvements in cognitive function tests, considerably smaller than reported in B vitamin and omega-3 DHADHA is short for Docosahexaenoic Acid. It is an essential omega-3 fatty acid found in fish such as salmon, mackerel and herring, and is often… trials. As an example, Solanezumab produced a slowing down of memory decline equivalent to a 1 point improvement on a 30 point memory test compared to placebo, while those on B vitamins had no further decline in memory at all.
Both ADU and Solenezumab produced no significant changes in clinical dementia rating. By contrast, in those given B vitamins with sufficient omega-3 status 70% ended up with a Clinical Dementia Rating of zero. A hands down win for B vitamins and omega-3 compared to amyloid drugs (see later).
Amyloid Drugs are a Busted Flush
According to Remi Barbier, founder of biotech Cassava, another player in the dementia drug space “The anti-amyloid approach has been the No. 1 approach for the past 25-30 years. It has failed repeatedly. Normally, when an approach fails, sometimes you try again. Certainly, three strikes and you’re out. It’s been 20 strikes and they’re still batting.”
Amyloid protein, along with tau protein, is a key regulator of brain homeostasis. During Alzheimer’s disease, amyloid protein formation occurs in parallel with disease progression, but that does not mean it is necessarily a primary contributor to pathogenic brain changes.
In mice, injecting amyloid protein improves MS-like symptoms, acting much like an anti-inflammatory agent. Tau protein, another target for drugs, may have a similar effect. It is only when these proteins become damaged that they can contribute to pathology in the brain. The important question is what damages them?
Amyloid and tau may simply be part of an anti-inflammatory response and blocking their formation appears not to be the solution. A parallel is the whole LDL cholesterolLDL is short for low density lipoprotein. It is the “bad cholesterol” which collects in the walls of blood vessels, causing blockages. High LDL levels… story. LDL cholesterol gets damaged, both by glycation (sugar and refined, junk food) and by oxidation (smoking, fried foods and lack of fruit and veg). Damaged LDL means LDL cholesterol levels go up. LDL cholesterol is not the problem. It’s a marker for the problem, which is why blocking cholesterol formation with statins is not particularly effective in stopping cardiovascular deaths. Not eating sugar and junk food, increasing antioxidants by eating more fruit and veg, supplementing vitamin CWhat it does: Strengthens immune system – fights infections. Makes collagen, keeping bones, skin and joints firm and strong. Antioxidant, detoxifying pollutants and protecting against… and magnesiumWhat it does: Strengthens bones and teeth, promotes healthy muscles by helping them to relax, also important for PMS, important for heart muscles and nervous… and not smoking is far more effective. Even more so if omega-3 rich seafood is included.
The same seems to be true with drugs that block amyloid formation. Amyloid is just a marker, not the cause of dementia, a fact underlined by the recent meta-analysis of 14 anti-amyloid drug trials that lowered amyloid but had no effect on cognition. The true extent of the failure of these drugs is likely to be much worse but researchers attempting to pool all of 34 trials were denied access to 20 of them.4 This is the same old story that has occurred with so many drugs, hiding the worst results to get the drug licensed to sell and to maximise profits.
The real solution to preventing Alzheimer’s lies in tackling the true underlying causes of brain changes caused by high levels of homocysteine and inflammation.
Dementia Drugs are Big Business
Treating and caring for people with dementia costs the UK over £35 billion a year. Every day 790 people are diagnosed with dementia – that’s the equivalent of seven double decker buses full of people. With an estimated 50 million sufferers worldwide dementia drugs are potentially very big business. Bringing an effective dementia drug to market is pretty much the last hope big pharma has for a blockbuster drug sellable to millions of people worldwide. (That was until covid came along.)
US government agencies pour $3.1 billion dollars a year into dementia research.5 UK government pledges somewhere around £100 million a year. But almost none of it is spent on true Alzheimer’s prevention, despite more than half the risk for Alzheimer’s being preventable factors we can change. Only 1% of Alzheimer’s cases is directly caused by genes.
Up to 2014 only £156,000 of UK government funds was spent on dementia prevention. Even today remarkably little is spent on nutrition and prevention of Alzheimer’s either by UK’s Medical Research Council or the Alzheimer’s Society or Alzheimer’s Research UK, all funded by UK government. The most obvious next step is a trial combining B vitamins with omega-3, given that both have shown clear benefit, not only on clinical ratings of dementia but reduction in the rate of brain shrinkage, far better than any drug to date. For the past five years Emeritus Professor of Pharmacology David Smith, former Vice Dean of Oxford University’s Division of Medical Science, one of the world’s leading experts in Alzheimer’s prevention, has tried and failed to get any further funding. In contrast, the total spend to date on failed Alzheimer’s drugs is likely to be closer to $30 billion.
With every hint of a positive drug trial result share prices sore, then crash with yet another failure. Despite previous negative findings for Biogen’s ADU some kind of re-analysis involving only those with the ApoE4 gene, (known to increase risk of Alzheimer’s by about as much as having a high homocysteine level), given 14 rounds of a high dose of the drug, is being presented to the FDA in the hope of achieving approval. Their ruling is expected on June 7th. Ten members of an advisory committee have voted against recommending its approval. One panelist was uncertain. None voted yes. The FDA isn’t bound by the panelists’ vote, but it often follows their recommendation.
However, much like the UK’s Medicines Health Regulations Authority (MHRA), itself largely funded by drug licence fees, there’s a revolving door of jobs between government officials and big pharma directors. There is big money at stake, in this case not only for the makers of ADU, Biogen, but other pharma companies (now re-branded as ‘biotechs’ to avoid the negative connotations of ‘pharma’). Dementia drugs pretty much represent the last chance for a blockbuster, a cash cow, which is why so many are now diversifying into vaccines as an alternative revenue stream to prop up flagging profits.
Whether or not it gets approved it is clearly nowhere near as effective as B vitamins and omega-3 given to those with raised homocysteine, which is the majority of those with dementia (see below). These nutrients have the added advantage of being free from adverse effects and relatively inexpensive.
Prevention is the Way is the Forward
Lack of B vitamins, primarily driven by poor absorption of vitamin B12, and lack of omega-3, a consequence of not eating seafood, are two out of eight major drivers of dementia. The others include a high sugar diet, a lack of antioxidants including vitamin C, good digestion, having an active mind and social life, physical activity, good sleep and less stress. Secondary risk factors are hypertensionHypertension is more commonly known as high blood pressure…., diabetes, depression and obesity, more often than not a consequence of these other primary drivers of cognitive decline. Most of these, too, are linked to inflammation. The existence of amyloid plaques and tau protein tangles are manifestations of inflammation in the brain, but not the cause. Inflammation is part of a pattern of disease called ‘metabolic syndrome’ that underlies every major 21st century endemic disease including arthritis, cancer, diabetes, depression, heart disease, obesity and strokes. None of these are well treated by drugs because drugs don’t tackle the underlying causes such as insulinInsulin is a hormone made by the pancreas. It is responsible for making the body’s cells absorb glucose (sugar) from the blood…. resistance and inflammation. All are a consequence, primarily, of changes to our diet, coupled with inactive lifestyle, stress and lack of sleep.
Of all these risk factors, having a high homocysteine, lowered by B vitamins, is the most evidence-based, probably the most important and very easy to change. That was the conclusion of a study of 396 studies on risk factors for the prevention of Alzheimer’s disease by Professor of Neurology at Shanghai’s Fudan University.6 Scientists at the US National Institutes of Health did a similar study of studies and attributed 22% of the risk of Alzheimer’s to raised homocysteine and a lack of B vitamins and 22% to a lack of seafood and omega-3.7
Omega-3 and B vitamins are a Dynamic Duo
The reason B vitamins and omega-3 are so important for mental health is easy to understand if you know something about brain cells (neurons) and how they are made. The critical membrane through which brain signals are passed, is made out of a specific kind of omega-3 fat called DHA, that has to attach to a phospholipid. DHA is 98% of the structural fat of the brain. Both DHA and phospholipids are rich in seafood. Phospholipids are also rich in eggs. But these two vital components of brain cells are actively bound together by a process called methylationMethylation is what occurs when the body takes one substance and turns it into another, so that it can be detoxified and excreted from the…. Methylation is dependent on B vitamins, especially B12, folate (found in greens and beans – think foliage) and B6. ZincWhat it does: Component of over 200 enzymes in the body, essential for growth, important for healing, controls hormones, aids ability to cope with stress… also has a vital role to play. If you don’t have enough a toxic amino acid called homocysteine starts to accumulate in the blood stream. So raised homocysteine = faulty methylation = need for more B vitamins. More often than not the critical deficiency is vitamin B12, found in fish, eggs, milk and meat. But the ‘deficiency’ is often not due to dietary deficiency as such but malabsorption triggered by a lack of stomach acid, made worse by antacid drugs, as well as the diabetes drug metformin and diuretics used for high blood pressure.
Even when B12 is poorly absorbed, if enough is given in high dose supplements, blood B12 levels rise, homocysteine levels fall and memory improves. Professor Smith’s study gave 20mg of B6 (ten times the RDA), 800mcg of folic acidWhat it does: Critical during pregnancy for the development of a baby’s brain and nerves. Also essential for brain and nerve function. Needed for utilising… (four times the RDA) and 500mcg of B12 (333 times the RDA) to people with pre-dementia, versus placebo. In those with raised homocysteine (>11µmol/l) the rate of brain shrinkage reduced by 53% and there was virtually no further memory loss in the majority of people in this landmark randomised placebo study published in 2010.8
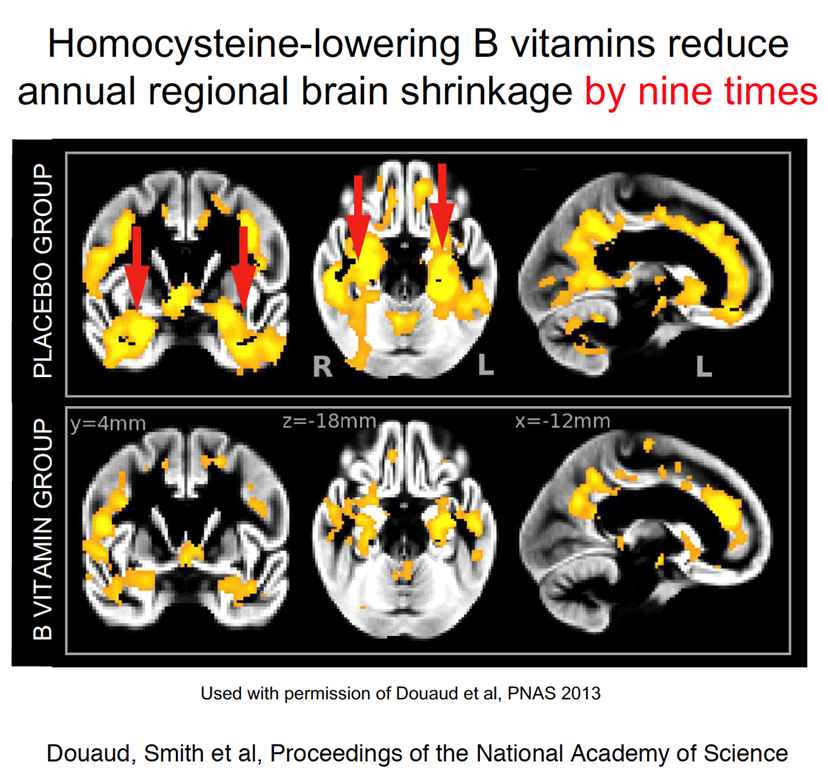
A later study looked specifically at the centralised areas of the brain where the most shrinkage occurs in Alzheimer’s.9 Those on the B vitamins had nine times less shrinkage.
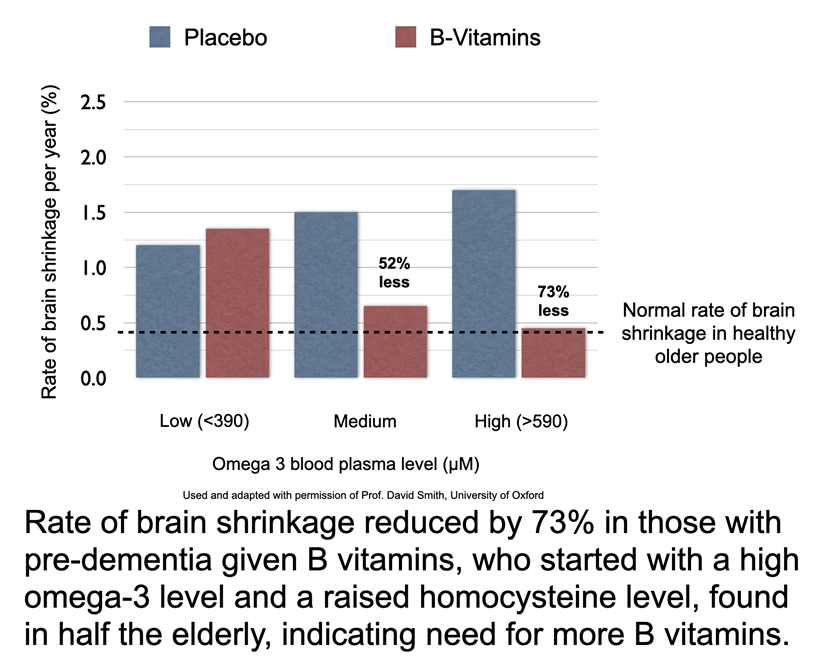
David Smith and co-researcher in his University of Oxford lab, Frederik Jerneren, wondered if the omega-3 status of their trial participants would have an impact of the B vitamin treatment. So they split the group into the third with the highest blood level of omega-3 down to the third with the lowest omega-3. To their surprise the B vitamin treatment didn’t work in those with low omega-3 status and vastly improved in those with sufficient omega-3. The rate of brain shrinkage over the year reduced by 73% in those sufficient in omega-3, given B vitamins, achieving the ‘normal’ level of age-related shrinkage seen in people without dementia and no measurable loss of cognitive abilities. What’s more memory loss ceased and 70% were classified with a Clinical Dementia Rating of zero, compared to 40% in the placebo group.10 That’s one third less rated with dementia. These results are leagues ahead of any drug, including ADU.
Several trials giving omega-3 fish oils or specifically DHA have shown clear benefits. Even something as simple as eating a serving of fish once a week has been shown to more than halve Alzheimer’s risk.11
A study of 65 healthy 50-75 year olds given 2.2g a day of omega 3 fish oils for 26 weeks not only showed improvement in cognition but also beneficial structural changes in white matter integrity and grey matter volume in the brain.12 The cognitive improvements tracked increases in blood levels of omega-3 and decreases in fasting insulin.
The obvious next step is to run a longer trial giving both omega-3 and homocysteine-lowering B vitamins to those with pre-dementia (called mild cognitive impairment or MCI). Such a trial would cost up to £5 million. Despite the billions of dollars spent on failed drug trials Professor David Smith has spent the last five years applying for funding – from the UK’s Medical Research Council, the Wellcome Trust, the EU’s Horizon fund and Australia’s NMRC to no avail. Tax-payers money is spent on drug trial research and genetics despite only one in a hundred cases of Alzheimer’s being directly caused by genes and no effective drug. It is money badly spent.
Modifying Genes with Nutrition
Even genetic risk factors such as having the ApoE4 gene variation, found in 25% of people, can be modified by the same kind of diet changes that reverse not only dementia but all the other ‘metabolic syndrome’ diseases. Eating a low GL diet, ketogenic diets, increasing omega-3 and antioxidants including vitamin C and quercitin, found in red onions, increasing B vitamins, vitamin D3 and K2 have all bee shown to mitigate the increased risk of genes and reduce Alzheimer’s risk.13
Why is Prevention and Nutrition being Ignored?
In a nutshell, the biggest problem for any prevention strategy, and especially one involving nutrients such as homocysteine lowering B vitamins and omega-3, is that there’s no big money to be made in naturally occurring nutrients because they can’t be patented. ‘If this was a patentable drug we could make billions’ the head of neuroscience in a major drug company told Professor David Smith. Without a patent you have no monopoly which allows you to charge as much as you like. Once the patent expires, as it has done for statins, the drug becomes ‘generic’ and cheap. That’s why biotechs are always looking out for the next thing to replace the drugs whose patents are expiring, even if it is, in reality, no better. A patentable drug, by its nature, has to do something unnatural, for example blocking an enzyme needed to make cholesterol or amyloid protein. This man-made interference inevitably means adverse-effects.
The B vitamin studies, like the drug trials, carried out on those with pre-dementia (MCI) have also been criticised because, despite showing much less abnormal brain shrinkage and no further memory loss, the trials weren’t long enough or large enough to conclusively prove the participants would not have gone on to develop Alzheimer’s. The B vitamin trial was for 24 months.
Yet, the hyperbole for the drug trials, worthy of the exact same proviso, instead are described as ‘the first drug to slow Alzheimer’s disease’.. ‘huge hope’ and ‘breakthrough in war on Alzheimer’s’. In truth, none of these drug trials can claim to prevent Alzheimer’s both because they haven’t arrested abnormal brain shrinkage, have little effect on clinical dementia rating and, even if they had ticked both these diagnostic boxes, suffer the same criticism of being too short to follow people for long enough – at least three to five years if the trials are large enough – to conclusively say the treatment prevents conversion from MCI to Alzheimer’s. The ADU trials were for 18 months, even shorter than the B vitamin trials.
The other way B vitamins get killed off is to give them to people who have no cognitive problem, no raised homocysteine level, and measuring cognition using a blunt instrument such as the MiniMentalStateExam (MMSE), comparing to placebo and showing ‘no change’. In other words, just giving B vitamins to healthy people doesn’t produce measurable changes in a basic test of cognition. These kind of studies are more politics than science but are widely quoted to prove that ‘B vitamins don’t work’.
Putting Prevention Into Action
There is no doubt that a number of factors under our control are driving the Alzheimer’s epidemic. These are:
• Lowering homocysteine with B vitamin supplementation
• Eating seafood and/or supplementing omega-3 DHA
• Avoiding sugar and following a low GL diet
• Increasing vegetables, fruits and antioxidants
• Keeping mentally and socially active
• Keeping physically active
• Building stress resilience and good sleep
• Promoting healthy digestion and microbiome
Changing these risk factors is the real goldmine for Alzheimer’s prevention. The gold is not in profits, but in saving people from this terrible fate that destroys not only their minds but puts a vast toll of their families. The real problem, however, is that change is not easy.
Also the sooner you make these changes the lesser will be your risk in later years. Subtle changes in cognition are measurable with a free on-line Cognitive Function Test, a fully validated digital version of what’s used in Memory Clinics, up to 40 years before a diagnosis of dementia or Alzheimer’s. Everyone over 40 should take this test.
The free Cognitive Function Test is offered by the charitable Food for the Brain Foundation. Over 360,000 people have taken the test, which also includes a questionnaire to assess your personal risk factors to advise you what simple actions will make the biggest difference.

Food for the Brain are now working with leading world experts, including Professor David Smith and Jin-Tai Yu not only in Alzheimer’s prevention, but also in effective behaviour change, to build a personalised, interactive, engaging ‘brain upgrade’ programme called COG-NITION® to encourage people to make positive changes step by step, with the support of an engaging and encouraging community. This is being funded by individuals like you, private donations, via a ‘Prevent Alzheimer’s Now’ Crowdfounder which gives more details of this landmark project that puts evidence-based prevention into practice. The crowdfunder goes live at 4pm (7 June) and donations made in the first 5 minutes are particularly effective, giving the appeal momentum – https://www.crowdfunder.co.uk/did-you-know-you-can-reduce-your-dementia-risk
The ultimate goal is to save a third of people from getting dementia which would mean 100,000 fewer cases a year in the UK alone. If they can raise £100,000 this will be ready in the Autumn. Please give whatever you can – every £1 you give literally helps someone somewhere make the changes to prevent Alzheimer’s disease. This disease is not an inevitable consequence of ageing, nor will it be cured by drugs. It is just another man-made disease, preventable with simple changes to nutrition and lifestyle, but sadly not reversible. That is why early prevention and education is the key.
References
1. https://pubmed.ncbi.nlm.nih.gov/33135381/
2. https://pubmed.ncbi.nlm.nih.gov/33632704/
https://www.bmj.com/content/372/bmj.n156/rr
3. http://www.biomedcentral.com/1471-2458/14/643
4. https://www.bmj.com/content/372/bmj.n156/rr
5. https://www.alz.org/news/2020/federal-alzheimers-and-dementia-research-funding-r
6. https://pubmed.ncbi.nlm.nih.gov/24962204/
7. https://pubmed.ncbi.nlm.nih.gov/24962204/
8. https://pubmed.ncbi.nlm.nih.gov/20838622/
9. https://pubmed.ncbi.nlm.nih.gov/23690582/
10. https://pubmed.ncbi.nlm.nih.gov/26757190/
11. https://pubmed.ncbi.nlm.nih.gov/12873849/
12. https://pubmed.ncbi.nlm.nih.gov/23796946/
13. https://doi.org/10.3390/nu13041362


Comments
Join the Conversation on our Facebook Page