In the UK an estimated 41,000 deaths, a third of the total of those dying within 28 days of a PCR positive test, were from people in care homes1, most of whom have both co-morbidities (other diseases), high oxidative stress (inflammation) and probably critically low vitamin CWhat it does: Strengthens immune system – fights infections. Makes collagen, keeping bones, skin and joints firm and strong. Antioxidant, detoxifying pollutants and protecting against… levels (the subject of our VitaC4Care study. An article in the British Medical Journal using numbers from the Office of National Statistics (ONS) attributed 47% of deaths in the first wave to care homes. 2 A study by the ONS attributes 59% of deaths to those who were disabled.3 Another estimates that 90% of those who died had significant prior poor health4
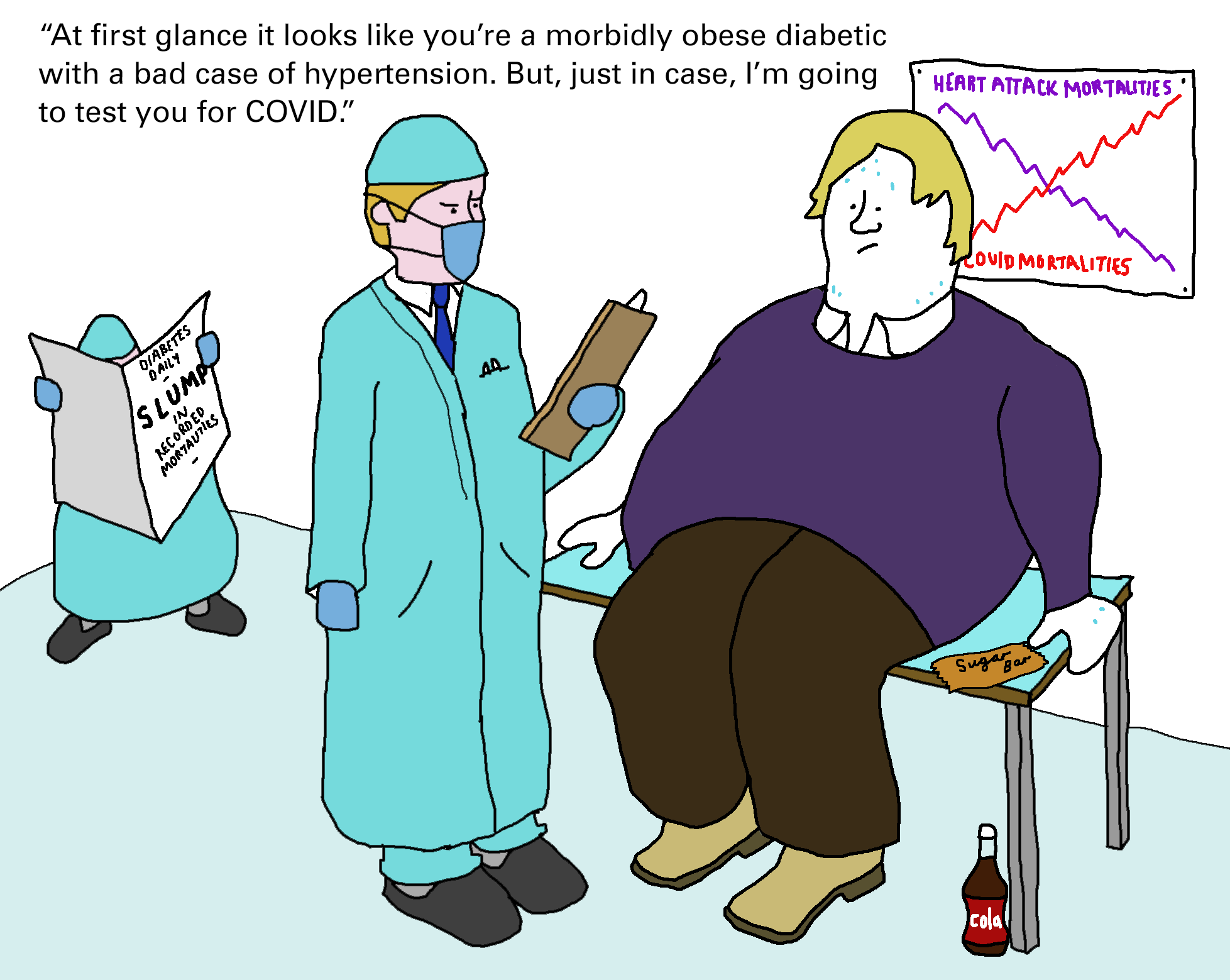
The UK has both the worst healthy life expectancy in Europe5 driven by obesity, hypertensionHypertension is more commonly known as high blood pressure…., chronic respiratory conditions, excess alcohol use, and inactivity. More people have died in Britain from COVID-19 as a proportion of its population than any other sizeable country.6
According to a recent article in the Lancet people with these problems are at greater risk of dying from covid. Obesity alone increases risk by 40%, according to Public Health England. 7“3·9 million people in Britain have diabetes and an estimated 4 million people have untreated hypertension. These risks and chronic conditions are more prevalent in people on low incomes and in poor communities, so more poor people die from COVID-19 than people on high incomes from wealthy areas.” reports the Lancet article.8
Every one of these risk factors is also associated with low vitamin C levels9 as are other known risk factors such as being older, male and african/american. Quite a few are also associated with lower vitamin DWhat it does: Helps maintain strong and healthy bones by retaining calcium. Deficiency Signs: Joint pain or stiffness, backache, tooth decay, muscle cramps, hair loss…. levels, especially skin colour. An estimated quarter of men and one in five women in the low-income/materially deprived population are also significantly deficient in vitamin C.10 In one Intensive Care Unit in Colorado, vitamin C levels not only predicted chances of survival. Age alone did not once vitamin C levels were taken into account.11
The Daily Mail reported that, according to NHS figures, just 388 healthy people under the age of 60, with no co-morbidities, died in England with a covid positive PCR test between April and December. It would probably have been even lower if people with low vitamin status had been excluded.
Vitamins that protect you from COVID-19
Vitamin C isn’t the only vitamin that you need more of as you age, and consequently are at greater risk of deficiency. It is, of course, vital for immunity with many roles to play in helping your immune defences fight off a virus.
Vitamin B12 levels also decline with age, but largely due to decreasing ability to absorb it rather than dietary deficiency. B12 is in fish, meat, eggs and milk. B12, together with vitamin B6, folate (from greens) and, to a lesser extent B2, B3 and zincWhat it does: Component of over 200 enzymes in the body, essential for growth, important for healing, controls hormones, aids ability to cope with stress… are all vital for a process called methylationMethylation is what occurs when the body takes one substance and turns it into another, so that it can be detoxified and excreted from the… that lies at the heart of how viruses replicate. Viral genes have to be inserted into a cell’s DNA and vaccines too, mimicking the viruses takeover bid, put a stress on methylation processes which uses up B vitamins, potentially promoting increased need and the risk of deficiency. Much like vitamin C needs go up when you’re fighting a viral infection, we cannot assume that a ‘well balanced diet’ does give you what you need when you’re under attack.
Low levels of vitamin B12 are associated with increased blood clotting12 and raised blood levels of the amino acid homocysteineHomocysteine is an amino acid found in the blood. Elevated levels of homocysteine have been associated with narrowing and hardening of the arteries, an increased… – a marker for faulty methylation – has long been linked with an increased risk of Alzheimer’s and heart disease. Recent research has found it also predicts the degree of lung damage in those with severe covid13and the risk of death14. Homocysteine levels, which tend to rise as we get older, are rarely tracked by doctors because the only way to lower levels is with very high doses of B vitamins.
So, could it be that the increased risk with age is more a function of a lack of vitamins B, C and D made worse by increasing prescription of antacids (PPI drugs) which make it harder to absorb B12 from food hence promoting deficiency?15 Most people over 70 are on at least five prescription drugs which lower or block the body’s ability to absorb vitamins.
Supporting the idea that raised homocysteine is a factor in covid damage is the fact that many of the classic symptoms of long covid mirror symptoms of faulty methylation and B12 deficiency16. These include strange sensations, numbness, or tingling in the hands, legs, or feet, difficulty walking (staggering, balance problems), anaemia, a swollen, inflamed tongue, difficulty thinking and reasoning (cognitive difficulties), or memory loss, weakness and fatigue. It’s required for healthy red blood cells so a lack leads to fewer red blood cells, leading to poorer oxygenation and breathing difficulties. A study giving vitamin B12 (500mcg) with vitamin D (1000iu) and magnesiumWhat it does: Strengthens bones and teeth, promotes healthy muscles by helping them to relax, also important for PMS, important for heart muscles and nervous… (150mg) resulted in less deterioration in older covid patients.17
The B12 link with clots and coagulation
What about the adverse vaccine reactions suffered by a relatively small number of people? In the case of the AstraZeneca vaccine these relate to problems with clotting and blood coagulation, a process that depends on B vitamins. My ears pricked up when a friend of my sister developed purple bruises all over his body following vaccination. ‘Purpura’ as this is called, is also a known symptom of B12 deficiency18. The thing about B12 is that it’s very hard to predict if you’re a malabsorber. A quarter of people with chronic B12 insufficiency take a decade to be diagnosed.
A UK study found that one third of people over 61 had insufficient B12 levels in their blood.19 B12 absorption requires good levels of stomach acid. The symptoms of low stomach acid include indigestion, bloating and heartburn. Tragically they are routinely treated with PPI antacid drugs that further inhibit B12 absorption making the situation worse.
It’s too early to know if vitamin or homocysteine status puts a person at greater risk of an adverse vaccine reaction but it is certainly something that should be studied, testing those that have had adverse reactions.
Last month I attended a meeting entitled ‘Levelling Health’ hosted by the All Party Parliamentary Group for Longevity. Both Matt Hancock and Sir Chris Whitty spoke about the importance of addressing the underlying causes of health disparity and the need to ‘health up’. Nutrition is probably the single most important aspect of this and the National Food Strategy, headed by Henry Dimbleby, has been set up to do this.
But somehow the ‘foodies’ don’t seem to get that what makes food good or bad for you is largely the presence or absence of nutrients such as vitamins and anti-nutrients such as refined sugar and carbs. Yet, somewhere in their group mindset is the idea that ‘you can get all the nutrients you need from a well balanced diet’ when the reality is that you cannot. The need to supplement with Vitamin D during winter is one example.
Another example of a dangerous nutritional deficiencies among older people is that 4% (an estimated 480,000 people) over 65 have overt deficiency levels of vitamin C20 as seen in those diagnosed with scurvy.
Our VitaC4care home study is the first ever to research how much vitamin C older people actually need just to have a normal level of vitamin C in their tissues. This sort of study should be welcomed, and funded by UK government, but the anti-vitamin mindset is so prevalent that some people wanting to give their parents in care homes vitamin C supplements have been told they cannot without their doctor’s permission. They should be thanked, not told off.
Hopefully, our VitaC4Care study will help shift this mindset. If you’d like to support this study – we need £20,000 and have raised £2,160 to date, please donate at www.vitaminC4covid.com .
REFERENCES
1. https://www.theguardian.com/world/2021/jan/19/covid-related-deaths-in-care-homes-in-england-jump; also see https://www.ons.gov.uk/file?uri=/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/numberofdeathsincarehomesnotifiedtothecarequalitycommissionengland/2021/20210419coviddeathnotificationsv1.xlsx
2. Oliver D. David Oliver: Let’s be open and honest about covid-19 deaths in care homes. BMJ. 2020;369:m2334
3.https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronaviruscovid19relateddeathsbydisabilitystatusenglandandwales/2marchto14july2020#overviewofcovid19relateddeathsbydisabilitystatus
4.https://static1.squarespace.com/static/5d349e15bf59a30001efeaeb/t/607d58172ad03b5b774f10d3/1618827288368/Levelling+Up+Health+Report+Digital+Final.pdf
5. GBD 2019 Viewpoint Collaborators. Five insights from the Global Burden of Disease Study 2019. Lancet 2020; 396: 1135–59.
6. Tallack C. Understanding excess mortality: comparing COVID-19’s impact in the UK to other European countries. The Health Foundation. 2020. https://www.health.org.uk/news-and-comment/charts-and-infographics/ comparing-covid-19-impact-in-the-uk-to-european-countries (accessed Dec 1, 2020).
7. Public Health England. Excess weight and COVID-19: insights from new evidence. 2020. https://www.gov.uk/government/publications/excess-weight-and-covid-19-insights-from-new-evidence (accessed Dec 1, 2020).
8. D Green, G Filkin, T Woods ‘Our Unhealthy Nation’ www.thelancet.com/healthy-longevity Vol 2 January 2021 https://doi.org/10.1016/ S2666-7568(20)30062-3
9. Patterson, G.; Isales, C.M.; Fulzele, S. Low level of vitamin C and dysregulation of vitamin C transporter might be involved in the severity of COVID-19 Infection. Aging Dis. 2020, 12.
10. Mosdol, A.; Erens, B.; Brunner, E.J. Estimated prevalence and predictors of vitamin C deficiency within UK’s low-income population. J. Public Health 2008, 30, 456–460.
11. Arvinte, C.; Singh, M.; Marik, P.E. Serum levels of vitamin C and vitamin D in a cohort of critically ill COVID-19 patients of a north American community hospital intensive care unit in May 2020: A pilot study. Med.Drug Discov. 2020, doi: 10.1016/j.medidd.2020.100064.
12. Wee, A. COVID-19’s toll on the elderly and those with diabetes mellitus – Is vitamin B12 deficiency an accomplice? Med Hypotheses. 2021 Jan;146:110374. doi: 10.1016/j.mehy.2020.110374. Epub 2020 Nov 12. PMID: 33257090; PMCID: PMC7659645; Can vitamin B12 be an adjuvant to COVID-19 treatment?
Lopes M et al GSC Biological and Pharmaceutical Sciences, 2020, 11(03), 001-005.
DOI: 10.30574/gscbps.2020.11.3.0155
13. Yang Z et al., Predictors for imaging progression on chest CT from coronavirus disease 2019 (COVID-19) patients. Aging (Albany NY). 2020 Apr 10;12(7):6037-6048. doi: 10.18632/aging.102999.
14. Ponti G et al, Homocysteine (Hcy) assessment to predict
outcomes of hospitalized Covid-19 patients: a multicenter study on 313 Covid-19 patients lin Chem Lab Med 2021; March 25 letter doi.org/10.1515/cclm-2021-0168
15. Lam JR, Schneider JL, Zhao W, Corley DA. Proton pump inhibitor and histamineHistamine is a chemical naturally produced by various cells in the body. A large amount of histamine is produced within mast cells where it forms… 2 receptor antagonist use and vitamin B12 deficiency. JAMA. 2013 Dec 11;310(22):2435-42. doi: 10.1001/jama.2013.280490.
16. McCaddon A, Regland B. COVID-19: A methyl-group assault? Med Hypotheses. 2021 Apr;149:110543. doi: 10.1016/j.mehy.2021.110543
17. CWen et al ‘Cohort study to evaluate the effect of vitamin D, magnesium, and vitamin B12 in combination on progression to severe outcomes in older patients with coronavirus (COVID-19)’Nutrition 2020, 79–80,111017, doi.org/10.1016/j.nut.2020.111017.
18. Severe vitamin B12 deficiency mimicking thrombotic thrombocytopenic purpura
Routh J et al Blood (2014) 124 (11): 1844. doi.org/10.1182/blood-2014-03-562488 ; see also Asano T et al., Neglect-induced pseudo-thrombotic thrombocytopenic purpura due to vitamin B12 deficiency. Pediatr Int. 2015 Oct;57(5):988-90. doi: 10.1111/ped.12718.
19. Vogiatzoglou A, Refsum H, Johnston C, Smith SM, Bradley KM, de Jager C, Budge MM, Smith AD. Vitamin B12 status and rate of brain volume loss in community-dwelling elderly. Neurology. 2008 Sep 9;71(11):826-32. doi: 10.1212/01.wnl.0000325581.26991.f2.
20. Bates B, Collins D, Cox L, Nicholson S, Page P, Roberts C, Steer T, Swan G. National Diet and Nutrition Survey Years 1 to 9 of the Rolling Programme (2008/2009 – 2016/2017): Time trend and income analyses. In: England PH, editor. London: Public Health England; 2019. p. 56

Comments
Join the Conversation on our Facebook Page