Hypnotized
In the UK over 80 million prescriptions are written out every year for psychiatric drugs, including addictive benzodiazepines, sleeping pills, mood stabilizers and anti-psychotic drugs. Most of these are numbing or hypnotizing drugs, suppressing emotions in a way not dissimilar to Aldous Huxley’s ‘soma’ in Brave New World.
Drugs, to be patentable, have to interfere with the body’s natural and multi-connected chemistry, often by blocking an enzyme or a receptor, as in the case of most antidepressants, which block the recycling channel or re-uptake channel for serotoninSerotonin is a hormone found naturally in the brain and digestive tract. It is often referred to as the ‘happy hormone’ as it influences mood…., or stimulant drugs for ADHD, which block the dopamineDopamine is a neurotransmitter (chemical messenger) found within the brain. It has a variety of influences on brain function including playing a role in regulating… receptor, thus mimicking slow-acting cocaine. The result can be a short-term boost in serotonin or dopamine, but a long-term depletion, leading to terrible withdrawal symptoms, including depression and hyperactivity – the very symptoms the drug was supposedly taken to cure.
Antidepressants are undeniably linked to increased risk of suicidal thoughts, among other adverse effects, including sexual dysfunction. Countries who prescribe the most have the most suicides.
Antidepressants are especially dangerous for older people as their less resilient chemistry is less able to deal with the drug. In a study published in the British Medical Journal involving over 60,000 people over 65 diagnosed with depression, among those given antidepressants there was one more death for every 28 people every year, compared to depressed patients not given antidepressants, and five times as many suicides. A recent review of 70 trials, also published in the British Medical Journal, found antidepressants double the risk of suicide and aggressive behaviour in under-18 year olds. The risk of suicide is especially strong when withdrawing from these drugs. The World Health Organization (WHO) rates three SSRIs as among the top 30 drugs for which dependence has been reported.
It is very difficult to get off most antidepressants, due to horrendous withdrawal-effects. Approximately four in 10 people have withdrawal symptoms, which can include depression. Doctors have no training in how to get people off the drugs they prescribe and tend to deny the seriousness of the situation. Among the most addictive are benzodiazepines and sleeping pills. Yet every year in the UK there are 16.5 million prescriptions for these drugs, and many for more than four weeks, which is the time needed to develop dependency. We have probably in the order of 4 million prescription drug addicts or dependents in the UK out of a population of some 60 million. Of course, all this is good for business.
Much of the marketing for psychiatric drugs is based on highly suspect research. For example, a seminal study in 2001, known as Study 329, concluded that antidepressants were both effective and safe for adolescents. Following the study, the UK’s biggest drug company, GlaxoSmithKline (GSK)’s sales of Paxil (paroxetine) rose to bestseller status in the USA, with sales of $340 million in the same year.
However, in 2004 GSK was fined $2.5 million for mismatches between their marketing claims and the data. The terms of the settlement included a requirement for GSK to post study results on the company website, including Study 329. In 2012 they were fined again, this time $3 billion – the biggest ever fine in corporate history. The next year paroxetine sales increased by 3 per cent.
Recently Study 329 has been shown to be nothing close to the truth. Using exactly the same data as the original study (obtained through an arduous process), an intrepid band of researchers came to exactly the opposite conclusion, namely that: ‘Neither paroxetine nor high-dose imipramine demonstrated efficacy for major depression in adolescents, and there was an increase in harms with both drugs.’ This re-analysis was published in the British Medical Journal.
It is extraordinary that in the UK there is not one public pressure group tackling this industry’s relentless pursuit of profits before lives. We have campaigns for animal rights, gay rights, civil rights and eco-rights and against war and tax-dodgers, but not one tackling the industry that is fined more than any other for illegal and immoral activities. In the UK, where Big Pharma’s influence goes deep into the government agency, the MHRA, responsible for protecting us, no fines have been issued, despite the very same violations being rampant as elsewhere in the world.
I am pleased to say, however, that there is a new professional group, the Council for Evidence-based Psychiatry, which at least has psychiatric drugs under the spotlight. I also have a campaign on avaaz.org9 with almost 5,000 signatures to date. Psychiatrist Dr David Healey, who first blew the whistle on the now established links between antidepressants and suicide, has done the most with his website rxisk.org, where patients and doctors can report and see adverse effects from drugs.
Professor Peter Gotzche, one of the key investigators for the independent Cochrane Collaboration, an international body which assesses medical research, calculates, in his book Deadly Psychiatry and Organised Denial, that deaths from psychiatric drugs are the third major killer after heart disease and cancer. Before you consider taking an antidepressant, I strongly recommend you watch his lecture on YouTube entitled ‘Why Few Patients Benefit and Many are Harmed’.
The Alzheimer’s Gravy Train
As a case in point, I’ve been watching the shenanigans on the biggest potential cash cow of all – Alzheimer’s disease. Alzheimer’s is now the most prevalent example of a breakdown in the brain’s ability to function in a connected way. Starting in the centre of the brain, the medial temporal lobe, brain cells (neurons) die off, leading to a progressive loss of cognitive function and, consequently, depression, confusion and frustration. Families struggle to cope with relatives who are affected. Most sufferers end up in care homes.
Already the healthcare cost of Alzheimer’s is more than that of cancer and heart disease combined. Left unchecked, Alzheimer’s will bankrupt our already failing healthcare system. So, the hunt for the miracle drug is relentless. Charities seek our money, pretending there is a drug cure is just around the corner. Political spokesmen make lame, unfounded predictions that by 2020 we will have it solved. Big Pharma has poured an estimated $50 billion to date into failed drug trials.
Yet no one is talking seriously about the ‘p’ word: prevention. The charity www.foodforthebrain.org has been campaigning for prevention to be taken seriously, given that half the risk for dementia is caused by things we can change, according to a consortium of 111 leading experts from 36 countries. Researchers at the US National Institutes of Health attribute almost a quarter (22 per cent) of Alzheimer’s cases to high homocysteineHomocysteine is an amino acid found in the blood. Elevated levels of homocysteine have been associated with narrowing and hardening of the arteries, an increased… levels, principally caused by a lack of B vitamins, and another 22 per cent to low seafood/omega-3 intake. (Our blood homocysteine levels reflect a vital process called methylationMethylation is what occurs when the body takes one substance and turns it into another, so that it can be detoxified and excreted from the….
Food for the Brain has raised over £80,000 for non-drug dementia prevention research and education. That is over half the total spend, £156,000, by all UK research councils from 2006 up to the end of 2013!14 The charity needs more funds! Please give generously.
To put this into context, the ‘best’ drug to date is Solanezub. The best non-drug treatment to date is B vitamins, given to those with raised homocysteine. B vitamins are especially effective in those with sufficient omega 3 – you need both to keep your brain healthy. The chart below shows you the comparative efficacy in the three critical aspects of Alzheimer’s: the rate of brain shrinkage, performance on cognitive tests, and clinical symptoms used for diagnosis.
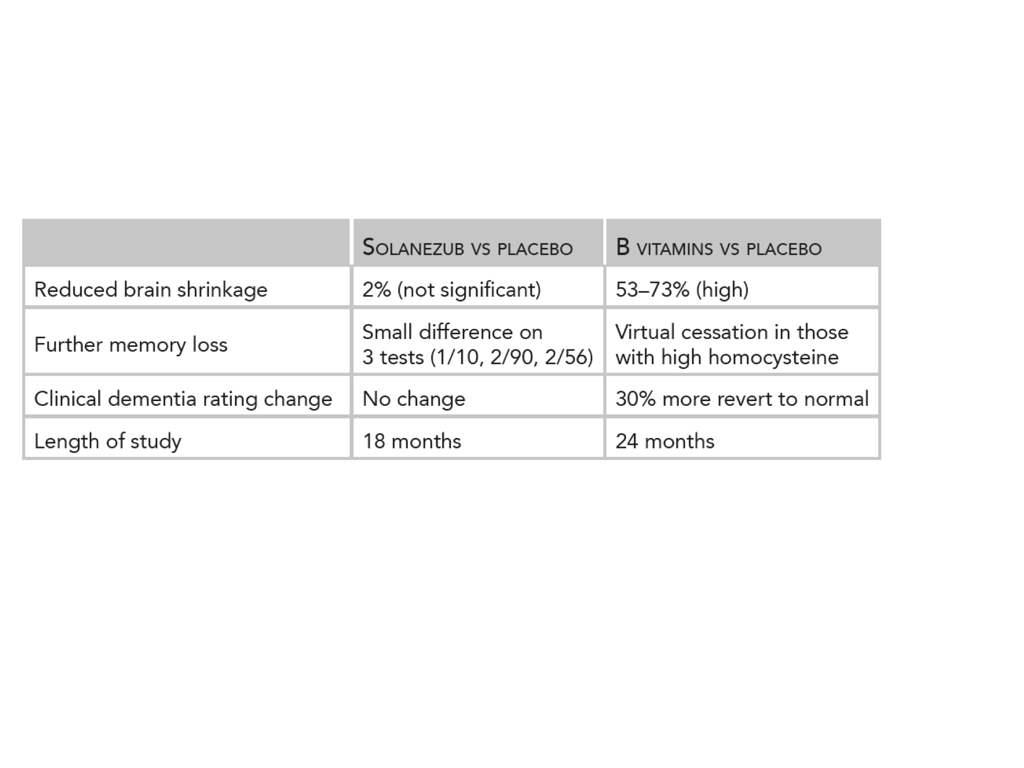 Comparison of best drug versus B vitamins on memory performance and brain shrinkage
Comparison of best drug versus B vitamins on memory performance and brain shrinkage
Prevention, however, is more likely to be given lip service until Big Pharma comes up with a drug to give to people under the guise of preventing dementia. The returns could be huge. So, they’d better bury this whole homocysteine and omega-3 story before it’s taken seriously. That’s how the game is played.
Burying the Cure for Schizophrenia
Another devastating disconnecting disease is schizophrenia, suffered by one in 100 people. Food for the Brain’s outpatient clinic, the Brain Bio Centre treats people suffering with schizophrenia not with drugs but by exploring their brain’s chemical imbalances and correcting them.
High homocysteine and a lack of B vitamins is a very common finding. We have over 50 years of research on the positive effects of B vitamins – niacin (B3), B12, folic acidWhat it does: Critical during pregnancy for the development of a baby’s brain and nerves. Also essential for brain and nerve function. Needed for utilising…, B6 and also zincWhat it does: Component of over 200 enzymes in the body, essential for growth, important for healing, controls hormones, aids ability to cope with stress… and magnesiumWhat it does: Strengthens bones and teeth, promotes healthy muscles by helping them to relax, also important for PMS, important for heart muscles and nervous… – often in high doses. Other common contributors to the disease are a lack of omega-3 fats and antioxidants, and also food intolerances. Some patients have neurotransmitterA neurotransmitter is a chemical messenger that carries signals between body cells. They are various types of neurotransmitters which play a major role in everyday… imbalances that can be made better with the right amino acidsAmino acids are commonly known as the building blocks of protein. There are 20 standard amino acids from which almost all proteins are made. Nine….
Many mental health concerns can be resolved by finding out what is out of balance and correcting it with nutritional medicine. According to a recent article in the Lancet medical journal, ‘Now is time for the recognition of the importance of nutrition and nutrient supplementation in psychiatry. Nutritional medicine should now be considered as a mainstream element of psychiatric practice.’
Instead, mainstream practice gives mind-numbing, usually patented and profitable drugs which, at best, stop a person harming themselves or others, but do not cure the disease. These drugs are ineffective in one third of patients and their side-effects can be severe and debilitating. They rarely improve the negative symptoms of the disease and long-term studies show better outcomes for those not medicated.
The sad truth is that most family members and people with schizophrenia do not know there are alternatives to drugs because the research has been buried, their psychiatrist doesn’t know either. T
here is a better way for mental health conditions, which combines enlightened psychotherapy and nutritional medicine. If there is a place for psychiatric drugs, it is as ‘holding’ drugs, such as tranquillisers to suppress overwhelming emotions when dealing with short-term crises, as one would do by getting drunk when overwhelmed with grief. However, these are best avoided except for very short-term use, as they carry the risk of addiction if taken beyond a couple of weeks.
Too many people have become hooked on antidepressants after being prescribed them for depression brought on by grief, losing a job or a marital breakdown. These are not good reasons to take drugs. There is no substitute for feeling and working through these deep emotions with the support of friends and a good therapist.
This excerpt is from Patrick Holford’s new book The Chemistry of Connection, which gives tools for enhancing connection. Patrick will be on a UK and Ireland tour starting next week talking about The Five Keys to Connection. For more details see www.patrickholford.com/connection.

Comments
Join the Conversation on our Facebook Page