What is an allergy?
To answer this question, you need to know a bit about your immune system. Inside your body is an army of immune cells on a 24-hour search-and-destroy mission. When they find an invader, such as a virus, they destroy it. The main way they capture their prey is by producing a tailor-made ‘straitjacket’ – an antibodyAn antibody is a protein produced by the body’s immune system when it detects a harmful substance known as an antigen. Examples of antigens include… – to fit a particular invader. This is how vaccination works – the polio vaccine exposes your body to the polio virus, not enough to make you sick, but just enough for the immune army to make polio antibodies, which are then in place to protect you in the future.
In the same way, if you’re allergic to pollen, when you breathe it in your body starts to produce antibodies to pollen. The most familiar symptoms of an allergy include hayfever, a stuffy and running nose, itchy eyes and skin, asthma, headaches, bloating, water retention and facial puffiness. These are signs that your body is trying to get rid of something it doesn’t like. Most allergic responses are inflammatory and can bring on pain, swelling and stiffness in the joints and muscles.
Classic food allergies involve the production of an antibody, called Immunoglobulin E (IgE), tailored to fit the offending food. IgE-based allergies produce immediate symptoms – such as a rash when eating seafood – and are thus quite easy to detect. However, many allergies involve IgG reactions. When you have too many IgG reactions occurring in your body symptoms develop. So your allergic reactions may only occur if you eat a lot of an offending food, or a group of offending foods together. Symptoms are therefore often delayed or hidden and thus harder to detect. Allergies to food are increasingly common.
The most common offenders are dairy products and grains, particularly wheat. However, many other foods cause reactions in some people. But why do some become allergic when others don’t?
Have you got leaky gut syndrome
An obvious place to start in unravelling the true cause of allergies is the digestive tract. After all, the lining of the gut is the first point of contact between foods and the immune system. Did you know that the intestinal lining alone is estimated to contain more immune cells and produce more antibodies than any other organ in the body? Hardly surprising then, that the intestinal lining and its immune system is an absolutely critical defence against food allergens and infections.
The gut can become more leaky, allowing incompletely digested food proteins to gain entry into the bloodstream. Research shows that people with food allergies do tend to have leaky gut walls.[4] Another possible reason is that your immune army may be malnourished and hence will over-react to harmless substances. Allergies are therefore much more likely to develop in people who have a weakened or over-reactive immune system, perhaps partly due to chronic inflammation or poor digestion. The likely allergens are foods eaten frequently, especially those that are potentially irritable to the digestive system.
Figure 13 – Foods most likely to cause allergy
| Food | Percent of Symptomatic Patients Affected by Food |
|---|---|
| *Corn | 56 |
| **Wheat | 54 |
| Bacon/Pork | 39 |
| Oranges | 39 |
| Milk | 37 |
| Oats | 37 |
| Rye | 34 |
| Eggs | 32 |
| Beef | 32 |
| Coffee | 32 |
| Malt | 27 |
| Cheese | 24 |
| Grapefruit | 24 |
| Tomato | 22 |
| Peanuts | 20 |
| Sugar (cane) | 20 |
* Corn is the most common in the US ** Wheat is the most common in the UK Data from: L G Darlington, ‘Dietary Therapy for Arthritis’, Rheumatic diseases clinics of North America, vol. 17 (2), 1991, pp. 273-85
As far as arthritis is concerned, the most common suspects are grains and dairy products, followed by pork, beef and eggs.
Some people also get relief by avoiding citrus foods and the nightshade family (which includes tomatoes, potatoes, peppers, aubergines and tobacco).
Our Deadly Bread
Although the average person eats between 100g and 200g of wheat every day, in the form of bread, cakes, pasta and cereal, it contains a gastrointestinal irritant called glutenGluten is a protein found in the cereals wheat, rye and barley. Obvious sources of gluten in the diet are bread, pasta, breakfast cereals and…, and is Britain’s number one allergenAn allergen is a substance that is foreign to the body and which can cause an allergic reaction in certain people. Pollen is an example…. Other grains, like rye, barley and oats, also contain gluten. These also cause allergic reactions in some people, as does corn (maize). However, rice, buckwheat, millet and quinoa are unlikely to cause allergic reactions.
According to Dr Hicklin, a consultant rheumatologist, grains are the most common allergen in rheumatoid arthritis.[5] He put 22 patients onto a diet excluding likely allergy-provoking foods. No less than 20 noted improvements in their symptoms. When tested with different foods, 19 reported that specific foods made them worse, most commonly grains. According to Dr Nadya Coates, a specialist in grain allergy at the Springhill Foundation in Oxfordshire, gluten has a structure that is alien to the body’s metabolismMetabolism is a term that is used to describe the chemical reactions that take place within the body’s cells. The body gets the energy it…. It sticks to anything and encapsulates smaller molecules, such as sugar, cholesterol, fats or minerals, which are then transported into the blood without being properly digested. Gluten, she believes, is the major obstacle in all digestive processes, with wheat gluten being the most toxic of all. Gluten is, unquestionably, an intestinal irritant. In highly sensitive people the lining of the small intestine, which consists of small protrusions called villi, becomes flattened. This is known as coeliac disease and leads to malabsorption, diarrhoea and loss of weight.
One recent study, published in The Lancet medical journal, found that almost half of people with rheumatoid arthritis showed gluten sensitivity while a quarter of those investigated also had damaged villi.[6] If you have any of the symptoms highlighted below, as well as joint pain or stiffness, a trial period off wheat, and possibly off all glutinous grains, is strongly recommended. 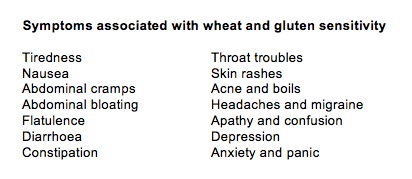 Milk Allergy
Milk Allergy
Milk allergy or intolerance is very common in rheumatoid arthritis sufferers. Consider the case, reported by Dr Panush, Professor of Medicine at the New Jersey Medical School, of a 52-year-old woman, who went on a three-day water fast, followed by a hypoallergenic (low allergy provoking) diet, excluding dairy produce.[7] Within 24 hours of starting the water fast there was noticeable symptomatic relief. She was then given capsules of foods to test. There were no noticeable responses to 52 placebos. Yet on the four separate occasions when she was given milk she reacted every time with a flare-up of symptoms and a raised blood ESR (a measure of inflammation).
Many similar reports of dairy allergy in arthritics have been published.[8] Sometimes reactions to dairy products are a result of lactose intolerance, since many adults lose the ability to digest lactose (milk sugar). The usual symptoms are bloating, abdominal pain, wind and diarrhoea, which subside on giving lactase, the enzyme that breaks down lactose. Probably equally common is an allergy or intolerance to the proteins in dairy produce. For reasons not yet completely understood, the most common symptoms are a blocked nose and excessive mucus production, respiratory problems such as asthma, and gastrointestinal problems. Such intolerances are more likely to occur in people who consume dairy products regularly, in large quantities. Some people who are intolerant of milk can tolerate yoghurt. Some can tolerate goat’s or sheep’s milk. Butter, which contains virtually no proteinProteins are large molecules consisting of chains of amino acids. Proteins are essential nutrients for the human body – they are a building block of…, is less likely to cause a reaction.
One Man’s Meat is Another Man’s Poison
Other animal proteins, particularly pork, beef and eggs, have also been noted to produce a worsening of arthritic symptoms in susceptible people.[9] Both vegetarian diets that include eggs and dairy products [10] and vegan diets, which exclude all meat, eggs and dairy produce [11], have produced positive results. One study followed 27 patients who started with a four-week stay at a health farm, where they were placed on a vegan, gluten-free diet which they followed for 3.5 months, then gradually moved to a vegetarian diet, including some dairy products and eggs.[12] Participants had remarkable improvements during the initial four weeks and were still showing benefit one year later.
Some arthritis sufferers seem to benefit from the exclusion of foods in the nightshade family (Solanaceae), which includes tomatoes, potatoes, aubergine, peppers and tobacco. This regime was made popular by Childers, a horticulturist, who found that this simple exclusion cured his arthritis.[13] Although unproven, these foods do contain solanum alkaloids which could theoretically inhibit normal collagen repair or promote inflammation. Other suspect foods include peanuts, oranges, grapefruit, malt and coffee. Coffee also appears to cause inflammation in the body, as shown by the presence of what are known as key inflammatory markers in the blood. A study involving over 3,000 people in Greece found that those consuming 200ml (7fl oz) of coffee – that’s two cups – had between 28 and 30 per cent higher levels of each of these kinds of inflammatory marker compared to non-coffee consumers.[14]
Inflammation is now recognised as the basis for many chronic degenerative diseases, including arthritis, so it makes sense to reduce unnecessary exposure to inflammatory agents, particularly when they are also slowing down the liver. I use a simple measure of the liver’s ability to clear caffeine from your system. This is a urine test that indicates how well your liver is detoxing.
Not everyone who has arthritis is allergic or sensitive to certain foods. So how do you know if you are? If you get three or more of the following symptoms, as well as joint or muscle aches, there is a good chance that you might be:
• hayfever
• a stuffy and running nose
• itchy eyes
• itchy skin
• asthma or difficulty breathing
• headaches
• bloating
• water retention
• facial puffiness
• discolouration around the eyes
If you eat any of the following foods most days and would find them difficult to give up, it’s worth testing to see if you’re allergic to them:
• wheat (bread, biscuits, cereals, pasta)
• dairy produce (milk, cheese, yoghurt)
• meat
• alcohol (especially beer and wine)
• coffee
• chocolate
• peanuts
• eggs
• citrus fruit
Pinpointing allergies or intolerances
The conventional way of testing for a food allergen is to avoid the suspect food then reintroduce it. A small percentage of food reactions involve an IgE based antibody, and cause pretty immediate reactions. If you have had a skin prick test this is an IgE based reaction. However, many food reactions involve a different kind of IgG antibody which doesn’t necessarily cause an immediate reaction so these delayed food reactions are not easy to pick up with an elimination diet. Also, using the elimination/reintroduction method you may not suspect the food, and so not test it. Or you may suspect only one food, yet be allergic to a range of them, so you’ll continue to have a background of allergic reactions.
The best and more accurate way to find out what you are reacting to is to have what’s called a Quantitative IgG ELISA test. This is the gold standard of allergy testing. ‘Quantitative’ means the test shows not only whether you are allergic, but also how strong your allergic reaction is. Many of us live quite healthily with minor allergies. But stronger allergies can create all sorts of problems, including weight gain. ‘ELISA’ is the technology used. You don’t need to know all the details but, trust me, it’s the most accurate system. If it’s done properly it is at least 93% reproducible. It’s used by almost all the best allergy laboratories in the world.
To convey why it’s so good, I need to explain a bit about the human immune system. Your immune system can produce tailor-made weapons that latch onto specific substances to help escort them out of your body. They are like bouncers on the lookout for troublemakers. The bouncers are called immunolobulins, or Ig for short. There are different types. The real heavies are called IgE, although most allergies involve IgG reactions. IgE reactions tend to be more immediate and severe. However, most ‘hidden’ allergies are IgG-based.
In an ideal world you test for both, but I normally start by testing a person for IgG sensitivity to food. All that’s needed for testing is a pinprick of blood, which is absorbed into a tiny tube and sent to a laboratory. The lab then sends back an accurate readout of exactly what you are allergic to. Your body doesn’t lie. You either have IgG bouncers tagged for wheat (for example) or you don’t. Your diluted blood is introduced to a panel of liquid food ‘testers’ and, if you’ve got IgG for that food, a reaction takes place. There are a number of laboratories who do IgG testing, and one that offers a handy test kit you can use at home. Yorktest have devised a clever procedure that involves a painless pinprick device and an absorbent material that you place against the pinprick. This material is then sent to the laboratory for testing (see yorktest.com).
The good news about IgG-based allergies is that if you avoid the offending food strictly for three to six months, the body forgets that it is allergic to it. The reason is that there will no longer be any IgG antibodies in your system to that food. So, provided you’ve removed the underlying cause of the allergy, such as intestinal permeability, and don’t over-eat that food every day, there’s a good chance that you won’t react to it any more. This doesn’t hold for IgE-based reactions, however. To give you an example, I have an IgE allergy to milk. I react within 15 minutes. Even if I avoid dairy products for a year, I still react if I consume one. I used to have an IgG to wheat. I avoided it for three months and now I no longer react. In my case, weight gain wasn’t the problem: it was migraine headaches. I had them every other week from the ages of six to twenty, until I discovered that wheat and milk were triggering them.
In summary, if you suspect you are allergic to something in your diet, you should:
• Work with your nutritional therapist to investigate any possible allergies or sensitivities.
• Get yourself tested with a reliable laboratory using IgG testing such as yorktest.com.
For more information about why allergies develop and how to prevent or reverse them, read my book Hidden Food Allergies with Dr James Braly.
REFERENCES
1. Royal College of Physicians report, ‘Allergy – Conventional and Alternative Concepts’ (1992)
2. Hardman G, Hart G, 2007: Nutrition and Food Science 37, 16-23
3. M. A. van der Laar and J. K. van der Korst, ‘Food intoleranceFood intolerance is not the same as a food allergy. Food intolerances tend to cause digestive symptoms such as bloating, cramps and diarrhoea, but are… in rheumatoid arthritis. I. A double blind, controlled trial of the clinical effects of elimination of milk allergens and azo dyes’, Annals of Rheumatic Diseases, vol. 51 (3), 1992, pp. 298-302; M. A. van der Laar and J. K. van der Korst, ‘Food intolerance in rheumatoid arthritis. II. Clinical and histological aspects’, Annals of Rheumatic Diseases, vol. 51 (3), 1992, pp. 303-306
4. T. Jalonen, ‘Identical intestinal permeability changes in children with different clinical manifestations of cow’s milk allergy’, The Journal of Allergy and Clinical Immunology, vol. 88 (5), 1991, pp. 737-42; see also N. Kalach et al., ‘Intestinal permeability in children: variation with age and reliability in the diagnosis of cow’s milk allergy’, Acta Paediatrica, vol. 90 (5), 2001, pp. 499-504
5. J. A. Hicklin et al., ‘The effect of diet in rheumatoid arthritis’, Clinical Allergy, vol. 10 (4), 1980, p. 463
6. C. O’Farrelly et al., ‘Association between villous atrophy in rheumatoid arthritis and a rheumatoid factor and gliadin-specific IgG’, Lancet, vol. 2 (8615), 1988, pp. 819–22
7. R. S. Panush et al., ‘Food-induced (allergic) arthritis. Inflammatory arthritis exacerbated by milk’, Arthritis and Rheumatism, vol. 29 (2), 1986, pp. 220–26
8. D. Ratner et al., ‘Juvenile rheumatoid arthritis and milk allergy’, Journal of the Royal Society of Medicine, vol. 78 (5), 1985, pp. 410–13. A. L. Parke & G. R. Hughes, ‘Rheumatoid arthritis and food: a case study’, British Medical Journal, vol. 282 (6281), 1981, pp. 2027–9
9. Marshall et al, Clin. Ecol., vol. 2, 1984, pp. 180–90
10. T. Sundqvist et al., ‘Influence of fasting on intestinal permeability and disease activity in patients with rheumatoid arthritis’, Scandinavian Journal of Rheumatology, vol.
11 (1), 1982, pp. 33–8 11. L. Skoldstam, ‘Fasting and vegan diet in rheumatoid arthritis’, Scandanavian Journal of Rheumatology, vol. 15 (2), 1986, pp. 219–23
12. J. Kjeldsen-Kragh et al, ‘Controlled trial of fasting and one-year vegetarian diet in rheumatoid arthritis’, Lancet, vol. 338 (8772), 1991, pp. 899–902
13. N. F. Childers & G. M. Russo, ‘The Nightshades and Health’, Horticulture Publications, Somerville, NJ, USA (1977)
14. A. Zampelas et al., ‘Association between coffee consumption and inflammatory markers in healthy persons: the ATTICA study’, American Journal of Clinical Nutrition, vol. 80 (4), 2004, pp. 862-7. A 50 per cent higher level of one of the markers (known as Interleukin 6), a 30 per cent higher level of another (known as C-reactive protein) and a 28 per cent higher level of a third (known as TNF) compared to non-coffee consumers.

Comments
Join the Conversation on our Facebook Page