But did you know that up to a fifth of an average GP’s salary is effectively commissions on drugs, on the basis that they decrease the NHS’s disease burden and consequently costs? However, the proverbial s**t is hitting the fan because a 10 year study has revealed that this vast increase in drug spend has done nothing at all to decrease NHS costs. To put this into numbers £30 billion has been spent rewarding GPs for prescribing drugs that have proven close to useless. And that money has come from your taxes.
Conducted in Britain, the largest-ever uncontrolled public health experiment ran for 15 years, cost £30 BILLION and found no benefits. The expectation was that it would save up to 30,000 lives a year, cut admissions to hospital and increase life expectancy, thereby reducing the costs of the NHS.
It didn’t do any of those, according to a report in the Lancet medical journal fulltext. The data the report was based on is something known as QOF (Quality and Outcomes Framework) which was a system set up in 2004 that started paying GPs for checking such biomarkers as blood glucose, triglycerides and cholesterol and then prescribing drugs to bring them down if they were over the official healthy level. They even get rewarded for identifying obese patients (but doing nothing about it.) ‘Our results show that the introduction of the QOF was not associated with significant changes in mortality for the diseases targeted by the program.’ reports the Lancet.
QOF bonuses account for between 8 and 20 per cent of a GPs salary, funded by your taxes –estimated as a £2000 annual tax bill for each household. In other words you, not the drug companies, effectively are paying the commission for prescribing ineffective drugs.
“At the start QOF was perfectly logical, if untried. The drugs, such as statins, blood pressure pills and diabetes drugs – had all been run through large randomised controlled trials which, it was widely accepted, showed they were effective and safe. It was believed that many people had undiagnosed risk factors, such as too much blood sugar or ‘dangerously’ raised cholesterol, so encouraging GPs to test and treat would inevitably improve the health of the nation and cut costs by reducing the number of people with diseases that needed expensive treatment. Wouldn’t it?” reports Jerome Burne, award-winning medical journalist, in his blog ‘the great QOF fiasco’.
Dr James le Fanu, columnist for the Times, has also blown the whistle on QOF and how it’s helped drive up drug prescriptions, in his new book Too Many Pills. In just fifteen years the number of prescriptions written by GPs has gone up three times, a rise which is implicated in the 75% increase in hospital admissions for adverse drug reactions between 1999 and 2008. The majority of these are elderly because they are more likely to be diagnosed as needing treatment – as we age, markers of ill-health such as cholesterol and blood pressure naturally rise – as well as being more likely to suffer ill-effects because their resilience naturally declines.
From 2000 to 2010 statin prescriptions went from 15 million to 70 million with no evidence of benefit for the elderly, says LeFanu. Writing in the Mail, LeFanu points out that a recent review concludes ‘Despite their widespread use, evidence for the effectiveness of statins in the elderly remains unclear.’ So far the only clinical trial in Britain that has specifically examined the drug’s effects in the elderly found that men were just 1 per cent less likely to have a fatal heart attack. There was no advantage for older women at all.’
Blood pressure pills emerge as a bit more effective – treating 2,400 people will prevent 50 strokes – which makes it worthwhile but there are no fewer deaths, most likely because of the rate of damaging side effects, such as badly damaging falls and an increased risk of diabetes, two side-effects associated with the drugs. According to LeFanu ‘The current medical practise of fetishizing numerical goals for blood pressure and the like, has led to an onslaught of drug treatments aimed at bringing people aged 60 and older into line with someone 30 or 40 years younger. The shocking truth is that the NHS is guilty of a terrible betrayal of our elderly — people who have trusted their doctors, without question, their entire lives.’ He is not the only medic who is feeling terribly let down. ‘It is frankly immoral to conduct policy in this way,’ says Tom Marshall Professor of Public Health and Primary Care at the University of Birmingham, referring to QOF and commenting on an article in the British Medical Journal headed ‘QOF “unlikely” to disappear in England but could be slimmed down’.
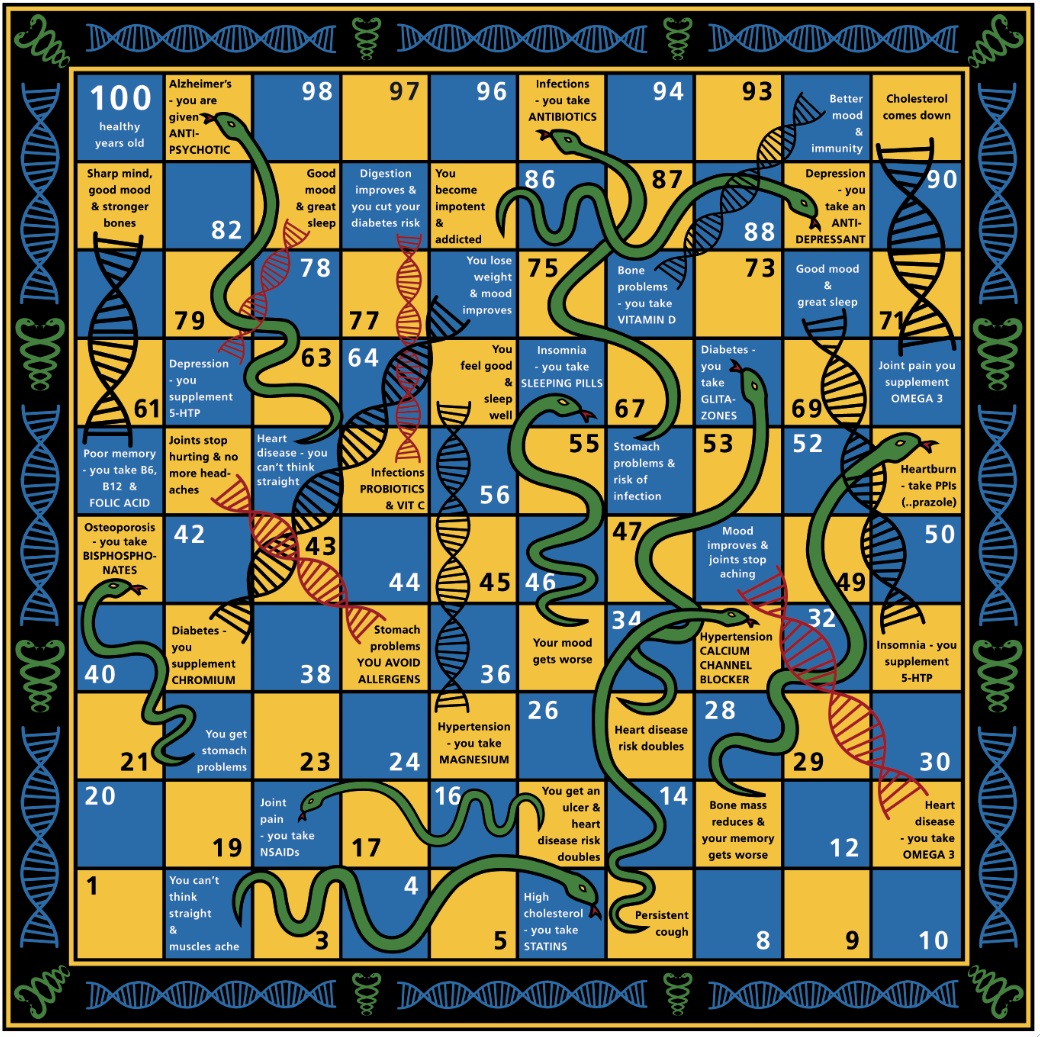
The Drug Cascade
Between 1995 and 2010, the proportion of UK adults getting five or more drugs doubled to 20%. Ten years ago, a year-long study on 100 nursing home patients found that stopping 320 of their drugs cut the yearly mortality rate from 45% to 21% and dropped hospital admission from 30 % to 11%. ‘A better result than achieved by any drug treatment anywhere,’ Le Fanu comments. Now 40% of US adults aged 65 years and over take five or more prescription medications. In the UK we are not far behind. Adverse drug reactions have been estimated as the fourth leading cause of death in US hospitals and are responsible for more than 700,000 hospital visits each year.
Professor David Healey, originator of rxisk.org, the website that gives the truth about drugs and their side-effects, blames over-prescribing on the fall in life expectancy, for the first time ever since the 19th century, in North America and Europe. “In the absence of any other explanation, the most likely reason has to be polypharmacy. More than five meds per day increases hospitalizations and shortens life spans. An increasing volume of evidence shows that deprescribing leads to fewer hospitalizations and increases life expectancy.” He has launched TaperMD.com, a project which supports doctors in helping their older adult patients reduce their medication burden and improve their quality of life. The skill of unprescribing is something GPs are neither taught nor remunerated. There are no payments for unprescribing, which my spellchecker tries to correct to ‘prescribing’. The word does not even exist.
There is a Better Way
In 2015 The Royal College of GPs called for QOF to be replaced so GP’s could do more holistic care. But nothing has been done about it. MPs generally have no idea about the QOF fiasco even if the medical profession is slowly waking up to this embarrassing and costly failure. The trouble is they don’t want up to a 20% cut in income, which is what would happen if QOF was abolished. According to Burne “QOF may very well be also blocking the introduction of more holistic, patient centred treatments that might very well be cheaper and more effective. If GPs really don’t know how best to keep us healthy and would need extra incentives to do it, that surely means a radical restructuring is needed and fast.”
One way would be for GP practices to employ a nutritional therapist and refer patients to them for more effective nutritional and lifestyle approaches. We now have several thousand registered nutritional therapists willing and able to work with GPs and clear evidence that nutritional medicine is cheaper, safer and more effective.
Jerome Burne and I wrote about this in Food is Better Medicine Than Drugs ten years ago, showing how nutritional medicine – diet and supplements – was already proven to be more effective, cost effective and considerably safer for the treatment of the chronic diseases that overburden the NHS. In that decade the evidence has just got stronger but the advice remains essentially the same. Since then I have met hundreds of people who have come up to me to express gratitude for having followed the advice in the book and reversed their health issue and consequently come off unnecessary medication.
What can you do?
- Educate yourself. Read one of my books about your chronic disease, and start to make nutritional and lifestyle changes.
- See a nutritional therapist. There’s a nationwide directory at www.bant.org.uk.
Say no to drugs. If you are offered ineffective drugs (Food is Better Medicine Than Drugs gives you the bottom line) just say no. The drug prescription might reward your GP through QOF, but it does not reward you. - Sign the petition. Help us get over 5,000 signatures to ‘Stop Drug Companies Putting Profit Before Lives’ at avaaz.org
- Tell your MP. Now the cat is out the bag, the experiment concluded and failed, we need an end to QOF and a radical rethink on how to educate and motivate GPs to do


Comments
Join the Conversation on our Facebook Page