Indicators that this is starting to happen are raised levels of various liver-related enzymes, the most commonly checked being AST, ALT, APT and GGT. If you’ve been told by your doctor that you have decreased liver function it is likely to be based on these test results. When your liver is making too much fatThere are many different types of fats; polyunsaturated, monounsaturated, hydrogenated, saturated and trans fat. The body requires good fats (polyunsaturated and monounsaturated) in order to…, AST and ALT spill out into the blood, so your level will go up. A raised level of APT or especially GGT indicates that your liver is being damaged or the bile duct is blocked.
Contrary to popular belief your liver is the organ that suffers most in diabetes, not your pancreas. According to Dr Jacqueline Paltis in the Sugar Control Bible, Johns Hopkins University found that in 5,000 diabetics autopsied only 2 per cent had a degenerated pancreas, whereas 98 per cent had damaged livers.
To put this into perspective up to 20% of the Western adult population is thought to have the first signs of poor liver function. For example, Dr David Unwin is a UK GP looking after 9,000 patients. 1,300, or 14%, had abnormal liver function tests, the vast majority of whom were overweight. There are no effective drugs for this condition. “For years I didn’t really know how to advise my patients, particularly if they said they didn’t drink much alcohol. Initially I wondered if they were telling the truth, but was it likely that so very many of them were lying?” says Unwin.
A low carb, low GL diet approach
He decided to investigate the effects of putting his patients on a low glycemic load diet. “I noticed I could predict which patients would have lost weight before they came into my consulting room from the improvement in GGT blood results alone- so began to wonder about raised GGT levels, diabetes and non-alcoholic fatty liver disease (NAFLD): Was dietary carbohydrateCarbohydrates are the primary source of energy for the body as they can be broken down into glucose (sugar) more readily than either protein or… a link?”
How effective is a low-GL diet for reversing abnormal liver function? David decided to investigate by tracking the progress of 69 patients with non-alcoholic fatty liver disease with an average GGT level of 77 iu/L (the normal range is 0-50) and an average Body Mass Index of 34.4Kg/m2 .Obesity is defined as having a BMI above 30 so these were obese patients for the large part. Patients were advised, and supported to follow a low carbohydrate diet, excluding sugar and sugary foods from their diet, but not fat.
After an average of 13 months on a lower GL/carb diet there was a 46% mean reduction in GGT of 30 iu/L, back into the normal range, accompanied by average reductions in weight of 9kg or 19lbs.1 Please note that the same kind of diet would be highly effective in alcohol induced liver damage but, of course, it is essential to eliminate alcohol.
Liver friendly foods and nutrients
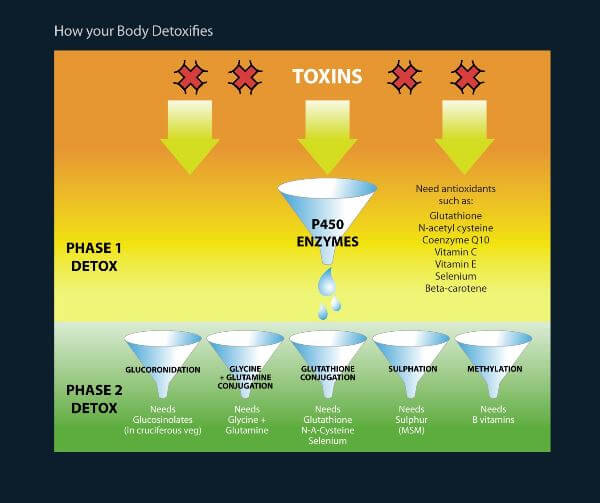
As you can see from the illustration above, the liver needs a wide range of nutrients to detoxify your body. The first phase of liver detoxification, which is required to detoxify both sugar and alcohol, depends largely on antioxidantAntioxidants are substances that protect cells within the body from damage caused by free radicals. They help to strengthen the body’s ability to fight infection… nutrients.
The second phase depends on other nutrients such as glucosinolates (found in cruciferous vegetables such as cabbage, cauliflower, kale, broccoli and Brussels sprouts); glycine (found in root vegetables); glutamine (found in tomatoes); glutathione and sulphur (present in onions and garlic, as well as eggs); and B vitamins (found abundantly in nuts, seeds, beans and greens).
There are a number of supplemental nutrients that accelerate a return to normal liver function. Glutamine is an interesting amino acid which can be used as fuel by some cells, notably in the gut and the brain, and it can also reduce sugar cravings. It has been shown to help lessen insulinInsulin is a hormone made by the pancreas. It is responsible for making the body’s cells absorb glucose (sugar) from the blood…. resistance and improve the function of the insulin-producing beta-cells in the pancreas.2 N-acetyl cysteine (NAC) is a precursor to making the key liver-friendly antioxidant glutathione, while SAMe helps make glutathione in the liver.
The herbs milk thistle (Silymarin) and turmeric (containing curcumin) are also really helpful in restoring liver function. Theracurmin, a particularly bio-available form of turmeric, has been shown to reduce the formation of acetaldehyde, a toxic by-product of drinking alcohol, by a third.3 To find out more about these nutrients and how to use them to restore liver function see my report on Protecting your liver from alcohol and recovering from Hepatitis C.
These nutrients are well worth supplementing in a detox programme, however these must be accompanied with a low GL detox diet. My book, The 9 Day Liver Detox Diet, including fabulous recipes from my co-author Fiona McDonald Joyce, is a great place to start since it gives you exact foods to eat, and supplements to take, for a rapid improvement in liver function.
Liver Detox Plan
Give your liver and digestive tract a break and your health a boost with thiscomprehensive one-week detox plan. Read More
References
- D.J. Unwin et al ‘A pilot study to explore the role of a low-carbohydrate intervention to improve GGT levels and HbA1c.’ Diabesity in Practice 4, 2015,
- J. R. Greenfield, et al., ‘Oral glutamine increases circulating glucagon-like peptide 1,glucagon and insulin concentrations on lean, obese and type-2 diabetic subjects’, American Journal of Clinical Nutrition, 2009; 89:106–13
- H.Sasaki H et al, ‘Innovative preparation of curcumin for improved oral bioavailability’ Biological and Pharmaceutical Bulletin 2011;34(5):660-5.

Comments
Join the Conversation on our Facebook Page